Translate this page into:
Complete Ophthalmoplegia: A Rare Presentation of Idiopathic Intracranial Hypertension
*Corresponding author: Vinod Khandait, Associate Professor, Government Medical College, Nagpur, Maharashtra, India. khandaitvinod@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal R, Khandait V. Complete ophthalmoplegia: A rare presentation of idiopathic intracranial hypertension. Vidarbha J Intern Med 2022;32:63-6.
Abstract
Idiopathic intracranial hypertension (IIH) is a disorder defined by clinical criteria that include signs and symptoms produced by raised intracranial tension (headache, papilloedema and vision loss), raised intracranial tension and normal CSF composition with no other cause of intracranial hypertension evident on neuroimaging. The most common symptom of IIH is headache; the most common sign is papilloedema and visual field loss. Here, we report a case of IIH which presented without headache, with visual loss and complete ophthalmoplegia in one eye and sixth cranial nerve palsy in other eye. There was no improvement in vision of patient on medical management and she was planned for a CSF diversion procedure. We highlight the various treatment options available for IIH and the importance of timely diagnosis and urgent treatment.
Keywords
Complete ophthalmoplegia
Idiopathic intracranial hypertension
INTRODUCTION
Idiopathic intracranial hypertension (IIH) is a clinical disorder of raised intracranial tension without a known aetiology. It is diagnosed when other causes of raised ICT are excluded from the study. Earlier called as benign intracranial hypertension to distinguish it from intracranial hypertension produced due to malignant neoplasm, it is no more referred to as benign disorder because it can lead to permanent visual loss.[1,2] Hence, the importance of early diagnosis and appropriate treatment has been stressed on. The pathogenesis of IIH largely remains unknown.[3] It is usually a diagnosis of exclusion when all other causes of raised ICT have been ruled out.[2,4] Here, we report a case of IIH presenting without headache, with external ophthalmoplegia in one eye and sixth nerve palsy [Figure 1] in other. We also discuss the various treatment options available in the disease.

- Complete ophthalmoplegia – left eye and ptosis – right eye.
CASE REPORT
A 22-year-old female brought by relatives with the complaints of heavy menstrual bleeding for 15 days back, for which she consulted a local general practitioner and was prescribed some medications. Five days later, she started complaining of poorly localised back pain and painless diminution of vision in both eyes accompanied by diplopia; followed by total loss of vision in both eyes for 4 days before admission. There was no history of trauma, fever, pain, watering or redness in eyes. There was no history of headache, vomiting, seizures or weakness of any side of body. There was no history of dysphagia, dyspnoea, loss of consciousness and ataxia. There was no past h/o hypertension, diabetes and tuberculosis.
On examination, her weight was 85 kg with height of 1.61 m and BMI of 32.8 kg/m2, BP 120/80 mmHg. Vitally stable. CNS examination: Normal higher mental functions. On Visual Acuity testing - there was no perception of light in both eyes. Fundus examination of both eyes revealed Frisen Grade 4 papilloedema. There was complete ptosis in the left eye with extraocular muscle movement restricted in all directions suggestive of 3, 4 and 6 cranial nerve palsy and partial ptosis is in the right eye with loss of abduction suggesting 6th nerve palsy. In both eyes, pupils were semi-dilated, not reacting to light. Rest of the CNS examination was normal. CVS, RS and PA examinations were normal. Investigations: CBC: Hb: 10.3, TLC: 11,000, RBC count: 3.81 million/cmm, PCV 30 and platelet: 347,000. LFT, KFT, Thyroid Function test were within normal limits, CRP was negative, Covid RTPCR was Negative, CSF.: Proteins- 28 mgm%, Sugar 58 mgm% With No Cells and Negative ADA. CSF manometry was done revealed CSF opening pressures of more than 25 cm of H2O. MRI brain with MR venography, MRI orbit and MRI spine was done. There was no evidence of hydrocephalus, mass or structural vascular lesion. Partially empty sella with pituitary gland flattened against the wall of sella, prominence of perioptic CSF space and subtle flattening of posterior sclera were seen, there was stenosis of the transverse sinus [Figures 2 and 3]. The patient was diagnosed as a case of IIH with external ophthalmoplegia on the basis of symptoms and investigations. As a part of treatment, intermittent lumbar puncture was done and 30 ml of CSF drained if CSF opening pressures were more than 25 cm of H2O and started on tablet acetazolamide at 250 mg bid with gradually increasing doses to maximum of 4 g/day in divided doses. Patient’s back pain was relieved and ptosis improved with full range of extraocular movements achieved; however, vision did not improve and repeat fundus examination was suggestive of both eyes papilloedema. The patient was posted for an urgent CSF diversion procedure.
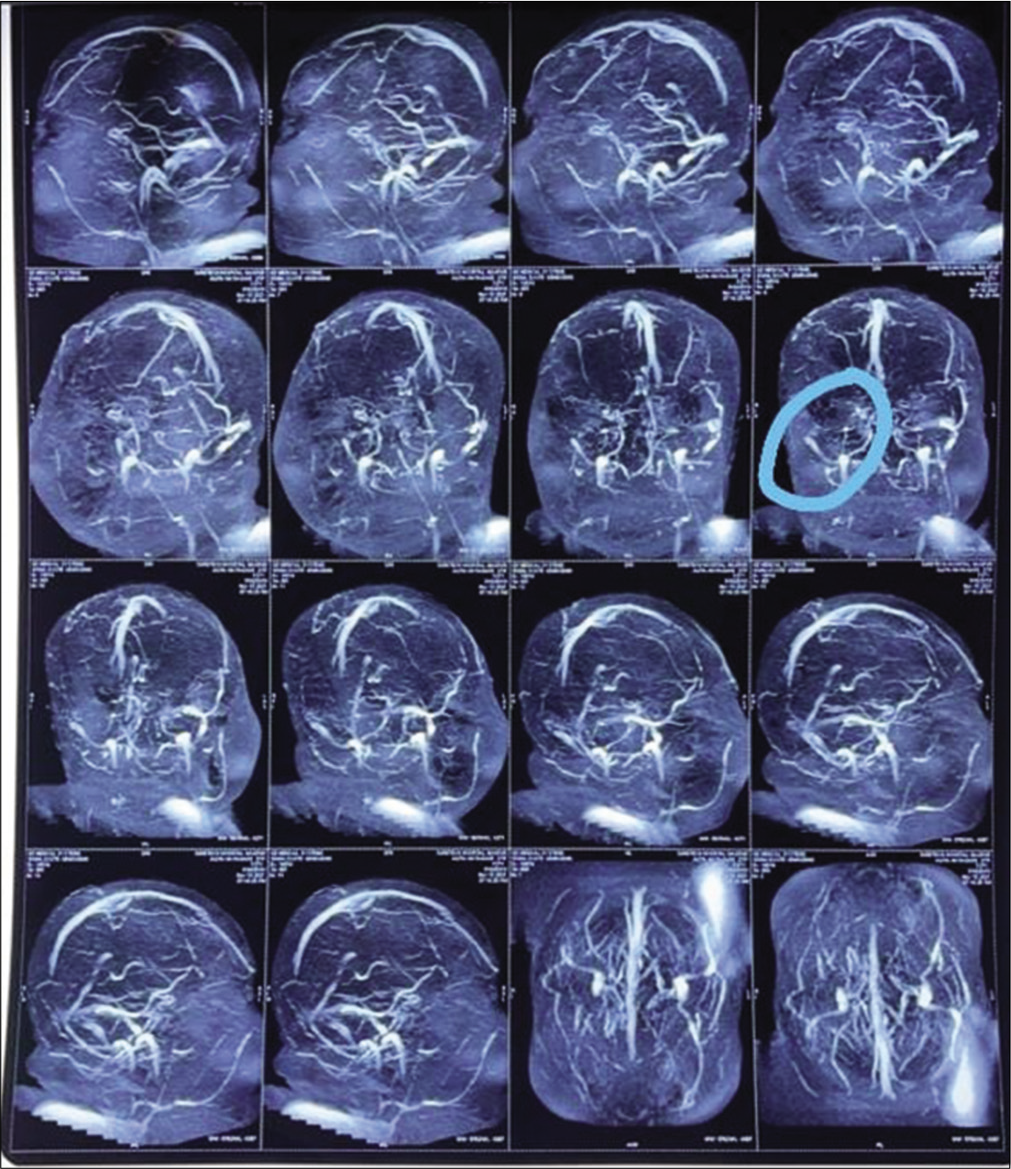
- Transverse sinus stenosis (showing on the left side in the circled area).
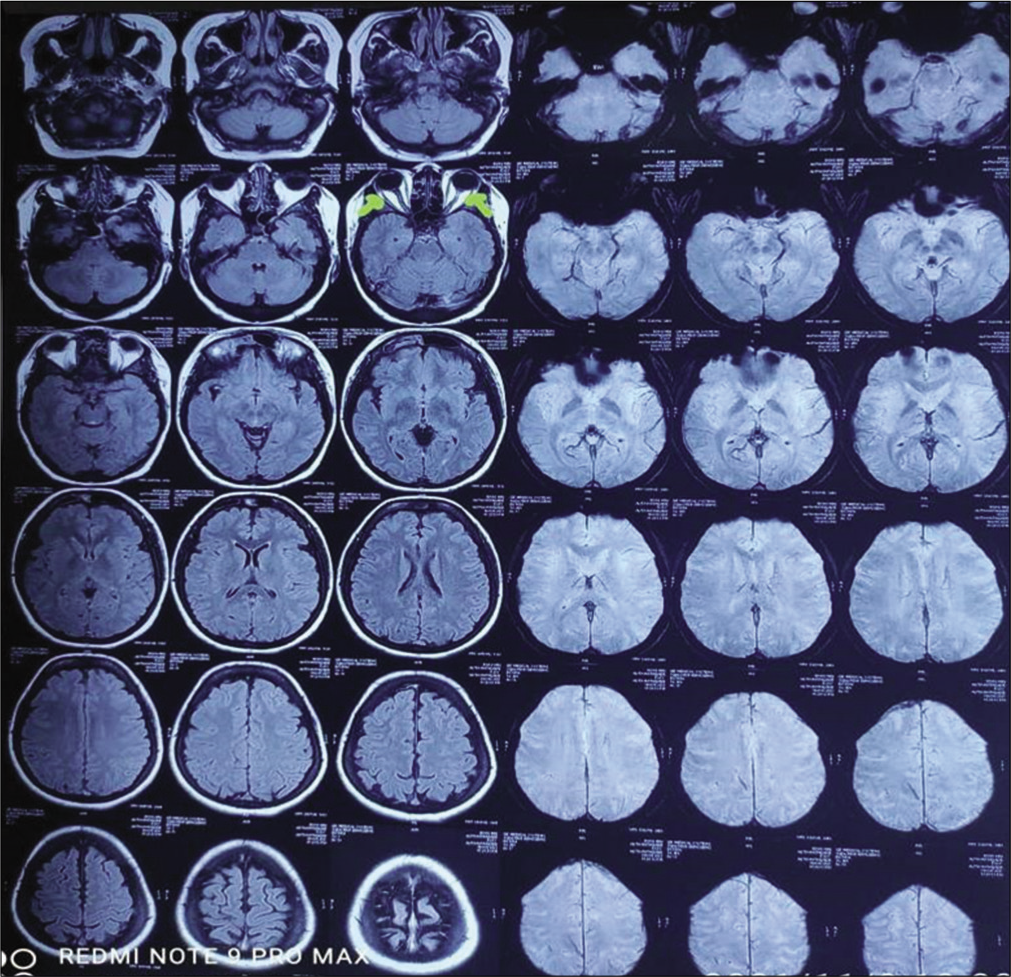
- Papilloedema and increased tortuosity of optic nerve.
DISCUSSION
IIH is a rare disorder with annual incidence of 1–2 per 100,000 population with the higher incidence noted in obese women of childbearing age. However, it can also occur in males, in children and in older patients.[1,5] Recent weight gain is a risk factor for IIH. Furthermore, a genetic component of IIH is suggested. By definition, IIH is idiopathic but a number of systemic diseases, drugs, vitamin deficiencies and excesses, anaemia and hereditary conditions have been reported. A link between IIH and menstrual irregularities, pregnancy, antibiotic use, iron deficiency anaemia, thyroid dysfunction and oral contraceptive use has been reported in studies.[2,3,6] Our patient presented with heavy menstrual bleeding before symptoms. Many medications have been associated with IIH including growth hormone treatment, retinoids and tetracyclines.[2] Systemic diseases including anaemia, polycystic ovarian disease and systemic lupus erythematosus have been linked to the disease but with uncertain pathogenetic mechanism.[2,6,7] The precise mechanism for IIH remains unclear. Venous sinus stenosis has been proposed as the cause of raised ICT. However, the most of the studies done point venous sinus stenosis is secondary to IIH and is not the primary cause of IIH. Other mechanisms proposed are increased CSF outflow resistance; obesity-related increased abdominal and intracranial venous pressure, altered sodium and water retention mechanisms and abnormality of Vitamin A metabolism.[2,4]
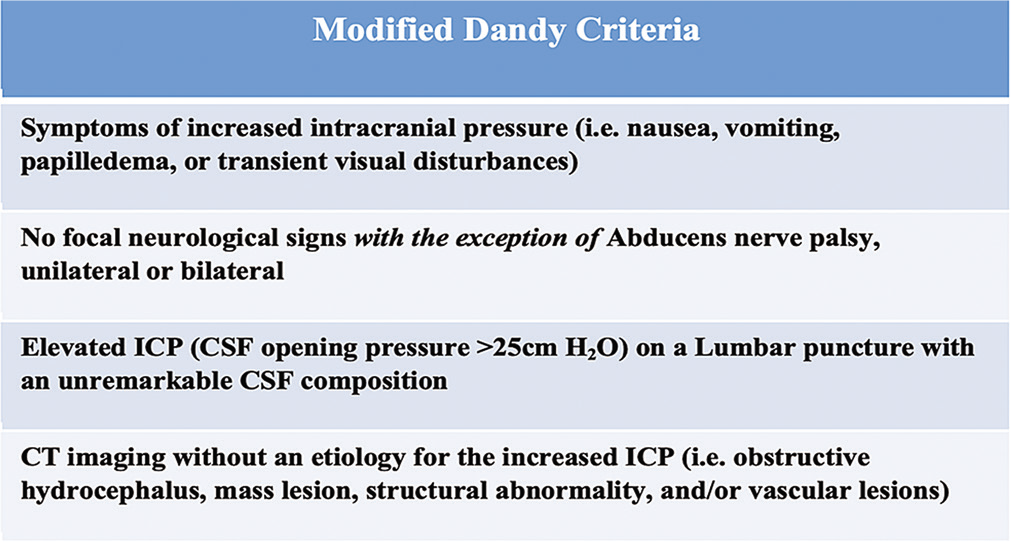
The most common symptom of IIH is headache. Headache is pulsatile, intermittent or persistent, associated with nausea-vomiting. Rare patients present without a headache and they carry a bad prognosis.[3] Our patient has presented without headache. Transient visual obscuration is reported in two-thirds of patients. A patient having more malignant or fulminant course presents with rapid development of vision loss which needs aggressive treatment.[7,8] Our patient presented with vision loss within 1 week of symptom onset. Horizontal diplopia due to the sixth cranial nerve palsy as a part of false localising sign is reported in 30% of patients.[3,9] Pulsatile tinnitus described as hearing rushing water or wind is a common symptom in IIH.[7] The most common signs in IIH are papilloedema, visual field loss and sixth nerve palsy.[8] Papilloedema is often bilateral and symmetric and the severity of visual loss depends on the grade of papilloedema. Other findings on fundoscopic examination include macular exudates and macular oedema and choroidal neovascularisation. Patients without papilloedema have been reported but are very rare. Loss of vision is the major morbidity in IIH and may present on initial evaluation as in our case. Visual field loss occurs before the loss of acuity.[8,10] The sixth cranial nerve palsy has been extensively reported in IIH but other cranial nerve deficits are rarely reported in the literature.[9] Our patient presented with total ophthalmoplegia. Landan et al. have reported in 1987 a case of IIH with complete bilateral ophthalmoplegia who recovered after optic nerve fenestration surgery. Kidron et al. have reported a case of young female of IIH who presented with rapid visual loss and ophthalmoplegia and was managed with lumboperitoneal shunt. We report a case of IIH which presented with complete ophthalmoplegia in one eye and sixth nerve palsy in other. The exact mechanism of cranial nerve deficits has not been clear but transmission of increased pressures to nerves have been proposed.[9] The diagnosis of IIH is made by modified Dandy criteria.[11]
MRI findings of IIH include flattening of posterior sclera, distension of perioptic subarachnoid space, empty sella and vertical tortuosity of optic nerve.[12] The treatment of patients with IIH has two major goals: The alleviation of symptoms and preservation of vision.[8,13] Risk factors for the development of visual loss are severe papilloedema at presentation, absence of headache, systemic hypertension, male sex, recent weight gain and higher opening lumbar pressures.[10] Any potential drug which can worsen IIH should be stopped. A low sodium, weight reduction program is recommended for all patients with IIH. Carbonic anhydrase inhibitors, acetazolamide, reduce the rate of CSF production and have been associated with modest outcome in IIH. Acetazolamide is started at low dose of 500 mg bid gradually increased to 4 g/day in divided doses. For patients who are unable to tolerate acetazolamide, furosemide can be started at doses of 20–40 mg/day. Rare patients who present with rapidly developing vision loss can be given a short course of steroids and serial lumbar puncture drainage. Less than 10% of patients may present with failure to respond to medical therapy or worsening of the symptoms despite maximum medical therapy.[4,8,14] These patients can be considered for intervention. The two main surgical procedures for IIH are optic nerve sheath fenestration (ONSF) and CSF shunting procedure. Cerebral venous sinus stenting is an alternative procedure.[13] ONSF is considered in patients having progressive visual loss. It has an efficacy of 94%. Complications of ONSF include efferent pupillary dysfunction from ciliary ganglion damage; visual loss can result from vascular complications. CSF shunting procedures include ventriculoperitoneal shunt or lumboperitoneal shunt.[15,16] Venous sinus stenting is a new and less researched procedure which needs further studies of its clinical benefit.[4] Most patients with IIH improve or stabilise with medical treatment over the course of several months; however, those presenting with rapid progression of symptoms and high grades of papilloedema are at risk of vision loss.[10]
CONCLUSION
IIH though presents with typical symptoms, it presenting as complete ophthalmoplegia is rare and only few cases have been reported. Timely diagnosis and urgent treatment is of paramount importance to save the vision. Hence, we report this rare presentation of IIH.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. Arch Neurol. 1988;45:875.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic intracranial hypertension. A prospective study of 50 patients. Brain. 1991;114:155.
- [Google Scholar]
- The idiopathic intracranial hypertension treatment trial: Clinical profile at baseline. JAMA Neurol. 2014;71:693.
- [CrossRef] [PubMed] [Google Scholar]
- Update on the pathophysiology and management of idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatry. 2012;83:488.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic intracranial hypertension (pseudotumor cerebri). Descriptive epidemiology in Rochester Minn, 1976 to 1990. Arch Neurol. 1993;50:78.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic intracranial hypertension: Report of seven cases. Am J Med. 1992;93:391.
- [CrossRef] [Google Scholar]
- Symptoms and disease associations in idiopathic intracranial hypertension (pseudotumor cerebri): A case-control study. Neurology. 1991;41:239.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of benign intracranial hypertension. Arch Dis Child. 1998;78:89.
- [CrossRef] [PubMed] [Google Scholar]
- Complete ophthalmoplegia: A rare presentation of idiopathic intracranial hypertension. Ann Indian Acad Neurol. 2015;18:468-70.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for poor visual outcome in patients with idiopathic intracranial hypertension. Neurology. 2015;85:799.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59:1492.
- [CrossRef] [PubMed] [Google Scholar]
- Magnetic resonance imaging in pseudotumor cerebri. Ophthalmology. 1998;105:1686.
- [CrossRef] [Google Scholar]
- Interventions for idiopathic intracranial hypertension. Cochrane Database Syst Rev. 2005;20:CD003434.
- [CrossRef] [Google Scholar]
- Non-operative management of benign intracranial hypertension presenting with complete visual loss and deafness. Pediatr Neurosurg. 2006;42:62.
- [CrossRef] [PubMed] [Google Scholar]
- Lumboperitoneal shunting for pseudotumor cerebri. Neurology. 1997;49:734.
- [CrossRef] [PubMed] [Google Scholar]
- Management of visual loss after optic nerve sheath decompression in patients with pseudotumor cerebri. Ophthalmology. 1995;102:441.
- [CrossRef] [Google Scholar]






