Translate this page into:
Severe Mitral Regurgitation: A Rare Manifestation of Chemotherapy-Induced Cardiotoxicity
*Corresponding author: Anil Ramesh Jawahirani, Department of Cardiology, Central India Cardiology Hospital and Research Institute, Nagpur, Maharashtra, India. anilramesh123@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jawahirani AR, Kalamkar RB, Washimkar SN, Chougule A. Severe Mitral Regurgitation: A Rare Manifestation of Chemotherapy-Induced Cardiotoxicity. Vidarbha J Intern Med. doi: 10.25259/VJIM_14_2024
Abstract
Chemotherapy has many side effects, and one which has deadly effects is cardiotoxicity. It can present as hypertension, myocardial ischaemia, arrhythmia, heart failure and thromboembolism. However, we hereby report a case of severe mitral regurgitation as a rare complication of chemotherapy.
Keywords
Mitral regurgitation
Cardiotoxicity
Chemotherapy
Complication
Side Effect
INTRODUCTION
Cardiotoxic side effects related to chemotherapy limit dosing and impose cancer survivors to enhanced morbidity and mortality.[1] Cardiac tissue is damaged in a variety of ways during cancer treatment.[2] The speculated mechanism of valvular regurgitation could be secondary to chemotherapy-induced reduced ejection fraction, but insufficient data favour this mechanism as a whole. Degenerative valvular regurgitation disproportionate to a decrease in the left ventricular ejection fraction (LVEF) and valvular or myocardial damage should be considered in survivors of chemotherapy survivors.[3] Current established guidelines for screening chemotherapy-related cardiotoxicity are mainly based on a serial assessment of the LVEF.[4]
CASE REPORT
A 57-year-old male who is a known case of acquired immunodeficiency syndrome with lymphoma, is taking antiretroviral therapy with chemotherapy for lymphoma and is in close follow-up, presented as an unscheduled visit on Sunday morning with complaints of fever, abdominal pain and cough and vomiting. He also had a history of a fall and trauma to the head and external bleeding without any evidence of head injury clinically and on a computed tomography scan. His last chemo drugs were vinblastine, doxorubicin, Holoxan, dexamethasone, Mesna, and Zofer. Ultrasonography revealed acute kidney injury and perinepheric hematoma. The patient also had abnormal kidney function test, liver function test and haemoglobin 3.2 g/dL. Chest X-ray was suggestive of pulmonary oedema. 2D echocardiography revealed severe mitral regurgitation (MR), with normal-sized left ventricle (LV) and normal LV function with no vegetation. Precise evaluation of the mitral valve showed no obvious cause for this severe MR, and severe MR was not secondary to left ventricular dilation or mitral valve annulus dilation [Figures 1 and 2]. The previous echo was done one month back after the fifth cycle was normal. Moreover, normal creatine phosphokinase-MB (CPK MB) and troponin T ruled out ischaemic heart disease as a cause of severe MR. Severe MR was so obvious that it led to consideration for its management as he needed a blood transfusion, cardiac support and dialysis and was shifted to critical care for further management, from where he took discharge against medical advice. His recent CD4 count is fair and viral load is undetectable.
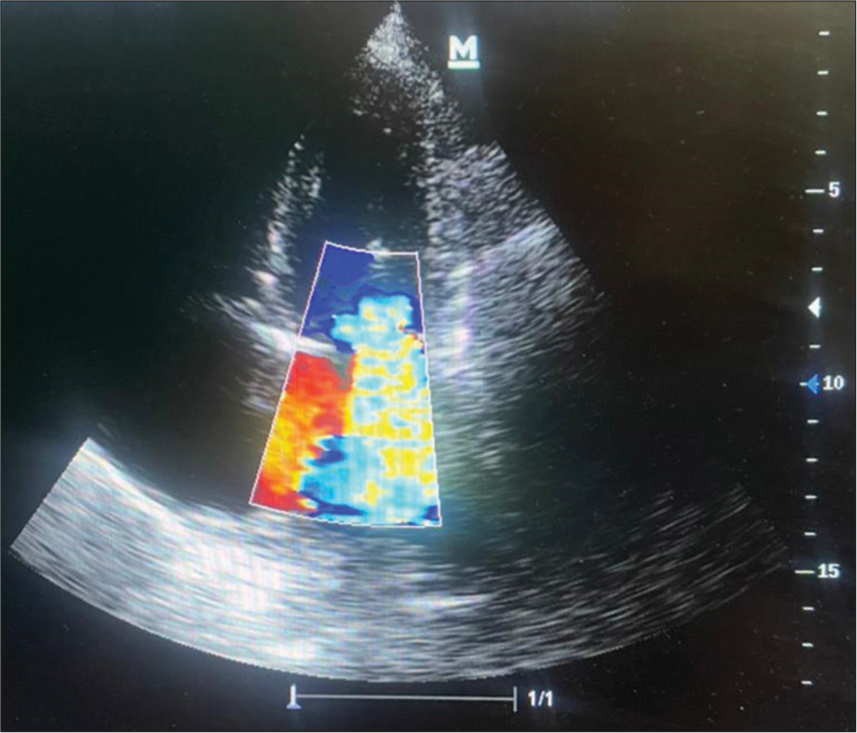
- Echocardiography showing severe mitral regurgitation in apical four-chamber view.
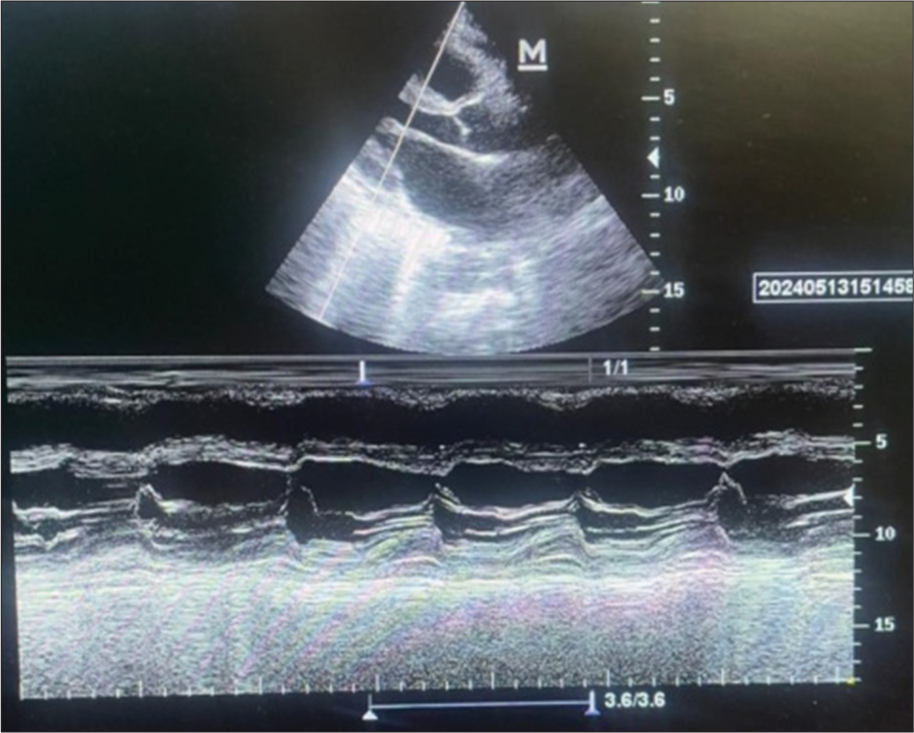
- Plax view in 2D echocardiography showing normal left ventricle volumes and function.
DISCUSSION
Hereby, we presented a case of severe MR, one of the rare presentations of chemotherapy-induced cardiotoxicity. There are only a few cases so far reported in the literature. Severe MR is a yet unreported manifestation of chemotherapy-induced cardiotoxicity which needs prompt attention. In one of the case reports, MR was reversible, similar to left ventricular dysfunction, which did not need an interventional and invasive strategy to manage it.[5] Since each chemotherapy agent has an impact on the cardiovascular system, cardiooncology knowledge should be joined from the beginning of patient management. The most likely cause is anthracycline-induced regional myocardial dysfunction which may be demonstrated as subclinical abnormalities in regional myocardial contractile function, despite normal LVEF.[6] In our case, there was no regional wall motion abnormality, and CPK MB and troponin test were normal, which rules out anthracycline-associated insult to the papillary muscle, like ischaemic myocardial injury, which may cause papillary dysfunction that impairs lateral shortening between the papillary muscles that tether the leaflet edges, leading to incomplete leaflet closure and significant MR, even in the absence of LV and mitral annular dilation.
Another explanation for the incipient MR is that the valvular ageing process may be accelerated by anthracycline toxicity. MR is seen in a considerable proportion of the general population and is thought to be related to ageing. Murbraech et al.[7] found that age >50 years at primary treatment was an independent risk factor for valvular dysfunction in lymphoma patients. In our case, MV thickening was not observed in the transthoracic echocardiographies (TTEs) after the onset of severe MR, which suggested that degenerative changes in the mitral valves did not play a role in the development of MR.
Mechanisms underlying anthracycline-induced myocardial damage are still less established. Proposed mechanisms include generation of toxic oxygen-free radicals, induction of apoptosis, inhibition of protein synthesis and DNA damage through interaction with topoisomerase II.[8] As exact mechanisms remain unclear, no specific agents that prevent anthracycline-induced cardiotoxicity have been developed yet. However, early detection and prompt treatment, as suggested by Cardinale et al.[9], are of great importance in the preservation and restoration of cardiac function, especially in patients with the onset of LVEF reduction occurring within first 12 months after chemotherapy.
Murbraech et al.[10] assessed the prevalence and associated risk factors for valvular heart disease in a cross-sectional national study of all adult lymphoma survivors after high-dose chemotherapy containing an anthracycline and autologous stem cell transplantation from 1987 to 2008. The 274 patients were compared with healthy age- and sex-matched controls. The mean follow-up after their lymphoma diagnosis was 13 years. Among those who only received an anthracycline, valve disease was seen in 17%, which was a three-fold increase compared with the controls and in 13% aortic valve degeneration was observed as compared with 3% in controls. Ventricular size was increased and function was decreased compared with controls, but these differences were modest. In those treated by chemotherapy only, age >50 years and ≥3 lines of chemotherapy were associated significantly with valve disease. The authors concluded that anthracycline-containing chemotherapy alone is associated with valvular heart disease due to valve degeneration. Ventricular function and left ventricular volumes were significantly different between chemotherapy patients and controls, but the changes were modest and of doubtful biologic significance, which suggests that myocardial toxicity was not the only explanation for the higher incidence of regurgitant valve disease in the chemotherapy alone group. In our case, ventricular function and volumes were preserved, signifying its rare manifestation.
CONCLUSION
Thus, severe MR without myocardial dysfunction can be a presentation of cardiotoxicity of chemotherapy. Thus, close attention should be paid to new-onset MR and increased efforts are needed for the early detection of cardiotoxicity, which is crucial to a timely change of chemotherapy regimen and an appropriate initiation of anti-remodelling therapy that could limit anthracycline cardiotoxicity and improve overall outcome.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Anthracycline Chemotherapy and Cardiotoxicity. Cardiovasc Drugs Ther. 2017;31:63-75.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Complications of Cancer Treatment In: Kufe DW, Pollock RE, Weichselbaum RR, Weichselbaum R, Bast R, Gansler T, eds. Holland-Frei Cancer Medicine (6th ed). Hamilton, ON: BC Decker; 2003.
- [Google Scholar]
- Valvular Dysfunction in Lymphoma Survivors Treated with Autologous Stem Cell Transplantation: A National Cross-sectional Study. JACC Cardiovasc Imaging. 2016;9:230-9.
- [CrossRef] [PubMed] [Google Scholar]
- Non-invasive Imaging and Monitoring Cardiotoxicity of Cancer Therapeutic Drugs. J Nucl Cardiol. 2012;19:377-88.
- [CrossRef] [PubMed] [Google Scholar]
- Severe Mitral Regurgitation, An Unusual Manifestation of Chemotherapy-induced Cardiotoxicity. J Res Med Sci. 2017;22:131.
- [CrossRef] [PubMed] [Google Scholar]
- Occult Cardiotoxicity in Childhood Cancer Survivors Exposed to Anthracycline Therapy. Circ Cardiovasc Imaging. 2013;6:873-80.
- [CrossRef] [PubMed] [Google Scholar]
- Valvular Dysfunction in Lymphoma Survivors Treated with Autologous Stem Cell Transplantation: A National Cross-sectional Study. JACC Cardiovasc Imaging. 2016;9:230-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anthracycline-induced Cardiomyopathy in Adults. Compr Physiol. 2015;5:1517-40.
- [CrossRef] [PubMed] [Google Scholar]
- Early Detection of Anthracycline Cardiotoxicity and Improvement with Heart Failure Therapy. Circulation. 2015;131:1981-8.
- [CrossRef] [PubMed] [Google Scholar]
- Valvular Dysfunction in Lymphoma Survivors Treated with Autologous Stem Cell Transplantation: A National Cross-sectional Study. J Am Cardiol Imaging. 2016;9:230-9.
- [CrossRef] [PubMed] [Google Scholar]






