Translate this page into:
A Case Report on Granulomatosis with Polyangitis and Diffuse Alveolar Haemorrhage
*Corresponding author: Dr. Vinod Vinayak Divakar, Department of Medicine, NKP Salve Medical College, Nagpur, Maharashtra, India. divakar.vinod33@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Divakar VV, Pande VK. A Case Report on Granulomatosis with Polyangitis and Diffuse Alveolar Haemorrhage. Vidarbha J Intern Med. 2023;33:101-3. doi: 10.25259/VJIM_13_2023
Abstract
Granulomatous polyangitis (GPA), formerly known as Wegener’s granulomatosis, is a rare form of small-vessel vasculitis. It has no gender predominance and tends to present between the ages of 40 and 55 years old in more than two-thirds of cases. GPA should be critically considered as a diagnosis when a presentation involves multiple systems, including joint, kidney, and lung. Lifesaving treatment of GPA is based on prompt and aggressive administration of pulse steroids and high doses of cyclophosphamide in repeat intervals.
Keywords
Granulomatosis with polyangitis
Small-vessel vasculitis
Multisystem involvement
Diffuse alveolar haemorrhage
INTRODUCTION
Granulomatous polyangitis (GPA), formerly known as Wegener’s granulomatosis, is a rare form of small-vessel vasculitis. It has no gender predominance and tends to present between the ages of 40 and 55 years old in more than two-thirds of cases.[1,2] The aetiology of the disease remains unclear, but there is a strong association with anti-neutrophil cytoplasmic antibody (ANCA).[3]
CASE REPORT
A 52-year-old female non-diabetic, non-hypertensive, presented with complaints of fever with chills for one month, haemoptysis one episode 1 month back, loss of weight and appetite for 15 days, and cough with expectoration for 15 days. On examination, the patient is conscious and cooperative, afebrile with vitals pulse - 130/min, blood pressure - 100/60 mmHg, respiratory rate - 18 pm regular, and oxygen saturation - 95% on room air. The patient had pallor. Respiratory system examination: Air entry bilaterally equal. Bilateral crepitations present till bases. Other systems were within normal limits. Complete blood count on admission was done: haemoglobin – 10.6 g/dL, total leucocyte count – 15220, PC – 346000, and mean corpuscular volume – 81.2, and liver function test and kidney function test were within normal limit. Erythrocyte sedimentation rate: 21, C-reactive protein: 239. Urine R/M: bacteria 7, RBC cast 6, blood cells 6. Sputum AFB and Gram stain tested negative. Truenat MTB: Not detected. c-ANCA: positive. Chest X-ray: suggestive of multiple cavitatory lesions along with surrounding lung consolidation [Figure 1]. High-resolution computed tomography (HRCT): multiple variable-sized thick-walled cavitary lesions with surrounding consolidation [Figure 2]. Multiple nodular and ground-glass opacities are noted. Vessels within these ground-glass opacities show a mosaic pattern of perfusion.
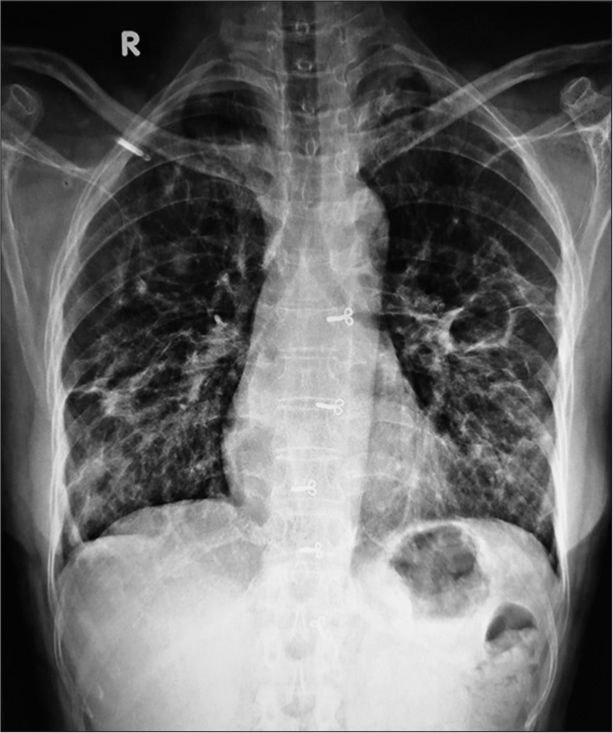
- Chest X-ray showing cavitary lesions. R: right..
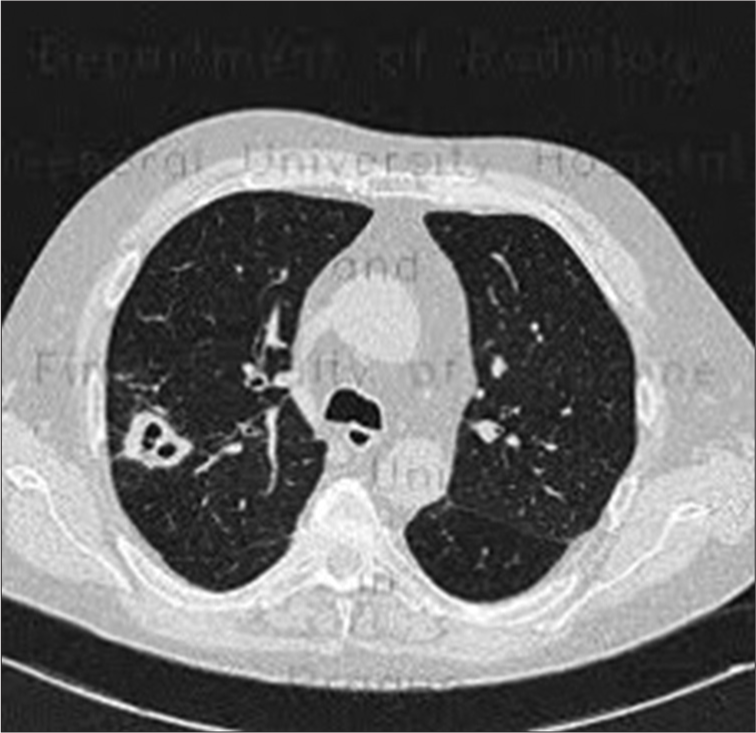
- High-resolution computed tomography (HRCT) chest image showing multiple cavitary lesions and ground-glass opacities.
Histopathology (HP 23395/96-23)
Linear bits of connective tissue showed many Langhans types of giant cells and scattered epithelioid cells. Moderate to dense inflammatory infiltrates, composed of lymphocytes and plasma cells, with focal areas of suppuration are present [Figure 3].
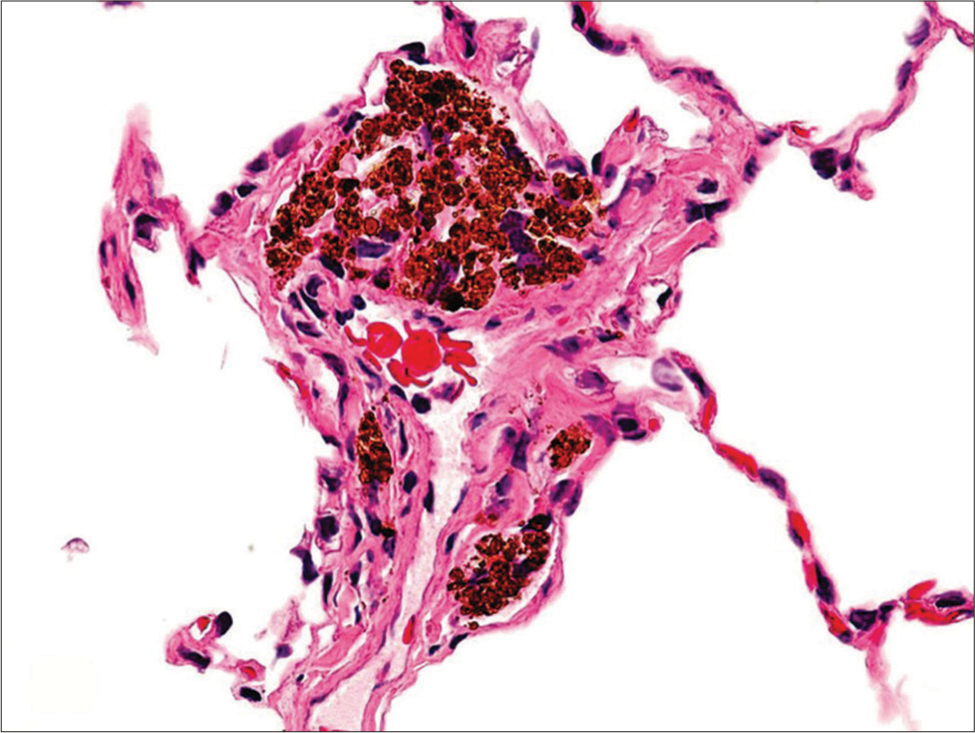
- Histopathology showing Langhans giant cells and inflammatory infiltrates.
Cytopathology (F-2376/23)
Many neutrophils, a few lymphocytes, and squamous cells are seen. Occasional endobronchial cells are seen as pigment-laden macrophages.
DISCUSSION
Based on the history and routine blood investigations, a diagnosis of pulmonary Koch’s was made; however, sputum AFB, Gram stain, and sputum CBNAAT tested negative. A fever profile was sent and tested negative. The patient still had persistent fever spikes (101–102°/day), and the patient suddenly desaturated and required 4–5 L of oxygen and had worsened on chest X-ray. HRCT was done patient had upper respiratory tract involvement (hearing loss, haemoptysis, and epistaxis), inflammatory polyarthritis, with constitutional symptoms of fever, weight loss, and nodulocavitary lung disease with diffuse alveolar haemorrhage. Hence, granulomatosis with polyangiitis with diffuse alveolar haemorrhage was suspected. ANCA antibody was sent, which tested positive. To further confirm the diagnosis, a CT-guided lung biopsy was done. The patient was given steroid pulse therapy injection of Solu-Medrol 1 g in 100 mL NS OD for three days with tablet Septran DS OD alternate day, tablet Waysolone 60 mg OD along with injection cyclophosphamide 600 mg in 250 mL NS over two h, three doses to be given three weekly followed by four doses at four weekly intervals.
CONCLUSION
GPA is a rare vasculitis affecting small vessels. c-ANCA with autoantibodies directed against proteinase-3 antibodies are seen in 80–90% of the cases with GPA, and the remaining are perinuclear-ANCA directed against myeloperoxidase antibodies. GPA involves multiple systems, including joints, kidneys, and lungs. Lifesaving treatment of GPA is based on prompt and aggressive administration of pulse steroids and high doses of cyclophosphamide in repeated intervals.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Wegener Granulomatosis: An Analysis of 158 Patients. Ann Intern Med. 1992;116:488-98.
- [CrossRef] [PubMed] [Google Scholar]
- 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65:1-11.
- [CrossRef] [PubMed] [Google Scholar]
- API Textbook of Medicine. Vol 1 and 2. (9th ed). Mumbai: The Association of Physicians of India; 2012. p. :146-58, 1339-42, 1695-750, 1868-75,1886-90
- [Google Scholar]






