Translate this page into:
Early Predictors of Success of Non-invasive Positive Pressure Ventilation in Hypercapnic Respiratory Failure
*Corresponding author: Gayatri Dhote, Department of Medicine, Indira Gandhi Government Medical College, Mayo Hospital, Nagpur, Maharashtra, India. dhotegayatri3@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Parate T, Dhote G, Parate R. Early predictors of success of non-invasive positive pressure ventilation in hypercapnic respiratory failure. Vidarbha J Intern Med 2022;32:3-9.
Abstract
Objectives:
To study the indication of NIPPV in patients with hypercapnic respiratory failure. To evaluate the clinical, laboratory and ventilatory parameters with respect to improvement or deterioration in general condition of the patient. To predict the outcome in the form of weaning from NIPPV or requirement of invasive ventilation. To compare APACHE II score with outcome.
Background:
Non-invasive ventilation (NIV) is now being considered more as the respiratory support of choice for acute respiratory failure. In some patients, with acute hypercapnic respiratory failure, NIV is inadequate and invasive ventilation is required for the management of respiratory failure. Thus, the determination of early predictors of the success of non-invasive positive pressure ventilation (NIPPV) is important to identify the patients who are likely to benefit from it. This study was done to determine the early predictors of the success of NIPPV in hypercapnic respiratory failure.
Material and Methods:
In the current hospital-based prospective observational study, 100 patients admitted with hypercapnic respiratory failure requiring ventilation therapy are included in the study. Baseline clinical (heart rate [HR] and respiratory rate [RR]), arterial blood gas (ABG) parameters (pH, pO2, and pCO2), and ventilatory parameters were recorded before the initiation of NIPPV. The above parameters were re-evaluated at 1, 4, and 24 h after initiation of NIPPV. Acute Physiology and Chronic Health Evaluation II (APACHE II) score was also calculated on admission and at the end of 24 h to compare with the outcome.
Results:
Of the 100 patients, 73% of patients showed improvement in clinical and laboratory parameters. There was an improvement in HR, RR, pH, pCO2, and pO2 within the 1st hour and continued to improve even after 1 h, 4 h, and 24 h of NIPPV in the success group. About 27% of patients who failed to improve required intubation. The optimum cutoff value for APACHE II score on admission for predicting the outcome of NIPPV was found to be 33 in this study. Therefore, a score above 33 predicts failure of NIV.
Conclusion:
This study demonstrated that the clinical and laboratory parameters predict the success of NIPPV in patients with hypercapnic respiratory failure averting the need for mechanical ventilation.
Keywords
Non invasive positive pressure ventilation
Hypercapnic respiratory failure
Mechanical ventilation
INTRODUCTION
The first -line treatment of patients with acute respiratory failure (ARF) is mechanical ventilation. Patients with ARF can be ventilated either invasively or non-invasively. Noninvasive ventilation (NIV) increases alveolar ventilation and reduces the work of breathing in patients with hypercapnic respiratory failure like chronic obstructive pulmonary disease (COPD).[1] Consequently, it reduces respiratory rate (RR), decreases PaCO2, and improves the level of consciousness.[2,3] It not only reduces the need for endotracheal intubation and its associated complications such as airway trauma, ventilator-associated pneumonia, and others but also reduces the complications associated with a stay in the intensive care unit (ICU), the length of hospital stay, and mortality in the selected group of patients.[4] The evidence for the use of NIV remains strongest in patients with hypercapnic ARF, due to exacerbations of COPD.[2,4]
In many patients, the application of NIV is insufficient as it does not obtain adequate ventilation, and eventually, endotracheal intubation and invasive mechanical ventilation is required for the management of respiratory failure. Furthermore, some patients may initially benefit from non-invasive positive pressure ventilation (NIPPV) but eventually deteriorate and require intubation. Patients who initially receive NIV but subsequently experience NIV failure and then receive intubation are in contrast to patients who initially receive invasive mechanical ventilation and are more likely to die in the hospital.[5,6]
Thus, it becomes important to ascertain the factors associated with NIV failure so that we can identify the high-risk subset of patients who are likely to fail a trial of NIV.
Aims and objectives of the study
The aims of the study were to study the indication of NIPPV in patients with hypercapnic respiratory failure, to evaluate the clinical, laboratory, and ventilatory parameters with respect to improvement or deterioration in the general condition of the patient, to predict the outcome in the form of weaning from NIPPV or requirement of invasive ventilation and to compare Acute Physiology and Chronic Health Evaluation II (APACHE 2) score with the outcome.
MATERIAL AND METHODS
This hospital-based prospective observational study was conducted in a tertiary hospital in Central India between January 2019 and September 2020. A total of 100 consecutive patients diagnosed with Type 2 Respiratory Failure in General Medicine and Respiratory Medicine ICU were considered for the study.
Among those who fulfilled inclusion and exclusion criteria and gave written informed consent were enrolled for the study after being informed about the risks and benefits of the treatment. Inclusion criteria were the patients diagnosed with type 2 respiratory failure.
Exclusion criteria set were pulmonary oedema, pneumonia, acute respiratory distress syndrome, pulmonary embolism, chronic pulmonary fibrosis, uncooperative patients, haemodynamic and cardiac instability (unstable angina and acute myocardial infarction), serious cardiac arrhythmia, unconscious patients, need for endotracheal intubation on admission to protect the airways or to manage respiratory secretions, inability to properly fit the facemask due to skeletal deformity and patients or their relatives not willing to give written informed consent.
Demographic data, history, clinical examination, and relevant investigations were recorded for each patient. NIV-BIPAP mode was used in all patients. Arterial blood gas (ABG) parameters (pH, PaCO2, and PaO2), clinical parameters (HR and RR), and ventilator parameters were recorded on admission, at 1 h, 4 h, and 24 h. APACHE2 score was calculated on admission and at 24 h. Patients who have deterioration of pH, increase in PaCO2, worsening of mental status, and intolerance to NIV were proceeded to invasive ventilation. Inspiratory positive airway pressure (IPAP) was initially set at 12 cm H2O and increased by increments of 2 cm of H2O up to 18 cm H2O based on clinical response and ABGs. The initial expiratory positive airway pressure (EPAP) was set at 6 cm H2O and was increased by 1 cm of H2O. Humidified oxygen limited to a maximal flow rate of 5 l/min using an oxygen connector on the face mask to achieve a level of arterial oxygen saturation above 90% on pulse oximetry was administered. Other treatments were provided for the different aetiologies as per standard protocol.
Ethical permission
The study was carried out after obtaining permission from the Institutional Ethical Committee. Written informed consent was obtained from all cases and assurance regarding the confidentiality of data was given.
Statistical analysis
Data were collected and compiled using Microsoft Excel 2018 and then analysed using Statistical Package for the Social Sciences 20.0 version and Epi Info software 7 by calculating frequency, percentage, and cross-tabulations between various parameters. A Chi-square test of significance was applied to test the significance of association wherever necessary. The paired t-test was applied for the comparison of variables at each step (admission, 1 h, 4 h, and 24 h). Suitable graphs, charts, and photographs were added. Qualitative data were represented in the form of percentages. Quantitative data were calculated using mean ± SD and/or median with range. P < 0.05 was considered statistically significant.
RESULTS
This is a prospective randomised study in patients with hypercapnic respiratory failure who needed NIV at admission. A total of 100 patients consecutive patients who were fitting in inclusion criteria were evaluated. We have studied their important clinical, ABG, and ventilatory parameters for 24 h to assess their correlation with the success of NIV. Out of 100 patients, 27 patients had deterioration on NIV and were intubated. They were included in the NIV failed group (Group 2, n = 27). Those who recovered with NIV are included in NIV successful group (Group 1). Following are the various characteristics of the two groups [Table 1].
| Group 1 NIV successful |
Group 2 NIV failed |
Total | |
|---|---|---|---|
| Number (n) | 73 | 27 | 100 |
| Mean age (years) | 60.24 | 57.8 | 59.6 |
| Male (n) | 50 | 19 | 69 |
| Female (n) | 23 | 8 | 31 |
| COPD | 60 | 20 | 80 |
| Bronchial asthma | 3 | 1 | 4 |
| Neuromuscular disorder | 5 | 3 | 8 |
| Obesity (OSA) | 5 | 3 | 8 |
| APACHE II (at admission) | 28.82 | 44.6 | 33.1 |
| APACHE II (at 24 h) | 23.89 | 47.15 | 30.17 |
| NIV days | 3.7 | 2 | 3.25 |
NIV: Non-invasive ventilation, APACHE II: Acute Physiology and Chronic Health Evaluation II, COPD: Chronic obstructive pulmonary disease
As we have seen, 73 patients (out of 100) were improved with NIV and 27 patients required invasive ventilation. Therefore, the success rate of NIV in our study was 73%. The mean age in our study population was 59.6 years. The mean age in Groups 1 and 2 was 60.24 and 57.8 years, respectively. The most of the patients (75%) were in the age group of 50–70 years in both groups [Figure 1].
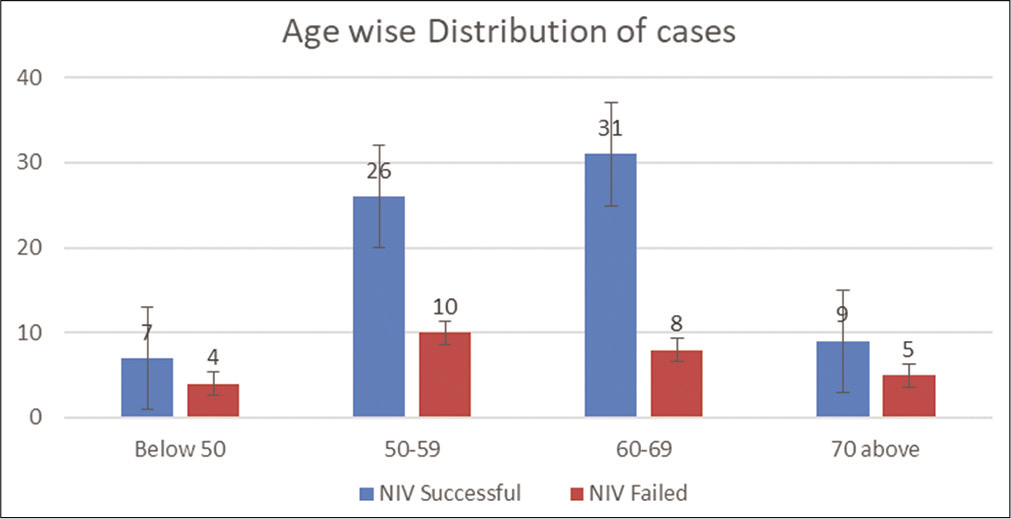
- Age group-wise distribution of patients.
There was no significant difference in outcome when age was considered [Table 2, P = 0.881]. In our study population, 69 male and 31 female patients were included in the study. In Groups 1 and 2, male preponderance was more (72% and 74%, respectively). When gender was considered, there was no significant difference in the outcome of NIV (P = 0.857).
| Total | Successful NIV | Failed NIV | ||||
|---|---|---|---|---|---|---|
| EPAP | IPAP | EPAP | IPAP | EPAP | IPAP | |
| Initial | 8.87 | 15.41 | 8.37 | 14.68 | 10.22 | 17.37 |
| 1 h | 8.61 | 15.15 | 7.79 | 14.04 | 10.81 | 18.15 |
| 4 h | 8.57 | 15.3 | 7.55 | 13.82 | 11.33 | 19.30 |
| 24 h | 7.88* | 14.55* | 7.08 | 13.39 | 11.8* | 20.2* |
Dyspnoea, as expected, was seen in all patients with respiratory failure. Other than that, the cough was the most common symptom (84%). It was mainly seen in COPD patients. The least common symptom was snoring (8%). It was associated with obstructive sleep apnoea in obese patients. Altered sensorium was seen in 11 patients with the high pCO2 levels.
COPD was the most common aetiology (80%) of hypercapnic respiratory failure in our study. Other less common causes are bronchial asthma, neuromuscular disorders, and obstructive sleep apnoea [Table 3]. NIV treatment was successful in 75% of patients with COPD and asthma. The success rate was about 62% with other aetiologies.
| Aetiology | Total | NIV successful | NIV failed |
|---|---|---|---|
| COPD | 80 | 60 | 20 |
| Bronchial asthma | 4 | 3 | 1 |
| Neuromuscular disorder | 8 | 5 | 3 |
| Obstructive sleep apnoea | 8 | 5 | 3 |
COPD: Chronic obstructive pulmonary disease, NIV: Non-invasive ventilation
However, statistically, the difference in outcome was not significant when aetiology was considered (P = 0.785) [Figure 2]. We did not find a statistically significant difference in days on NIV treatment when different aetiologies were considered (P = 0.163).

- Aetiology and days on non-invasive ventilation.
Heart rate (HR), RR, pH, pO2, and pCO2 were studied for all cases at admission, at 1 h, 4 h, and at 24 h. The following table shows the trends in these parameters with time [Table 4 and Figure 3]. We can see the improvement in all the parameters in the first 24 h.
| Variable | Mean (SD) | |||
|---|---|---|---|---|
| Basal | 1 h | 4 h | 24 h | |
| pH | 7.1 (0.03) | 7.2 (0.02) | 7.27 (0.04) | 7.29 (0.05) |
| pCO2 | 73.4 (4.9) | 67.1 (5.03) | 56.9 (8.4) | 46.9 (11.5) |
| pO2 | 63.6 (4.2) | 67.7 (3.04) | 75.4 (6.9) | 79.3 (6.8) |
| HR | 131.3 (3.5) | 123.06 (4.06) | 112.6 (4.2) | 106.1 (7.9) |
| RR | 33.5 (3.4) | 29.3 (4.2) | 25.5 (4.7) | 23.52 (5.6) |
HR: Heart rate, RR: Respiratory rate

- Clinical and ABG parameters (Groups 1 and 2).
In NIV, EPAP and IPAP levels were selected as per the need and they were changed from time to time. We have compared mean EPAP and IPAP levels at different times in Groups 1 and 2. We have observed that the requirement of EPAP and IPAP levels was progressively decreasing in Group I (successful NIV) and progressively increasing in Group 2 (failed NIV).
We have compared the variables at different times with the use of a paired t-test [Table 5]. There was no significant change in pO2 and pCO2 in the 1st hour in failed NIV cases.
| Successful NIV | Failed NIV | ||||
|---|---|---|---|---|---|
| Variable | t-value | Significance | Variable | t-value | Significance |
| HR | 25.64 | 0.001 | HR | 0.132 | 0.896 |
| RR | 14.28 | 0.001 | RR | 0.497 | 0.624 |
| pH | –18.36 | 0.001 | pH | –6.39 | 0.001 |
| pO2 | –28.58 | 0.001 | pO2 | –15.86 | 0.001 |
| pCO2 | 92.68 | 0.001 | pCO2 | 13.15 | 0.001 |
| EPAP | 4.35 | 0.001 | EPAP | Could not be done as12 patients are intubated before 24 h | |
| IPAP | 3.63 | 0.001 | IPAP | ||
EPAP: Expiratory positive airway pressure, IPAP: Inspiratory positive airway pressure, NIV: Non-invasive ventilation, HR: Heart rate, RR: Respiratory rate
Other changes in parameters are at a significant level. The changes in EPAP and IPAP were in opposite direction in successful and failed NIV case. Comparison using a paired t-test of variables at 1 h and after 4 h of NIV treatment was done. In this period (1–4 h), the changes in all the parameters were at a significant level in both groups. Again, the change in EPAP and IPAP was in opposite direction. Comparison using paired t-test of variables at 4 h and after 24 h NIV treatment.
In this period (4–24 h), the changes in HR and RR are not found significant (P = 0.896 and 0.624, respectively). The changes in all other parameters are at a significant level in both groups. Twelve patients were intubated before 24 h, and hence, paired t-test could not be applied to EPAP and IPAP in failed NIV cases.
We have calculated the APACHE II score for all patients. APACHE II score is considered to be a good indicator of patients’ clinical assessment. We have compared the APACHE II score at admission and 24 h for both the groups. In Group 1 that is successfully treated with NIV, the APACHE score was significantly reduced in 24 h. In Group 2 which is failed NIV cases, the APACHE score was significantly increased in 24 h [Figure 4].

- Comparison of Acute Physiology and Chronic Health Evaluation II score in Groups 1 and 2.
Greater scores suggest worse condition and poor prognosis. We can notice from the following figures that the more the APACHE II score at admission, the more are the chances of failure of NIV (or need for invasive ventilation) [Figure 5].

- Acute Physiology and Chronic Health Evaluation II score at admission and outcome of non-invasive ventilation.
We have considered the number of days of NIV in failed (Group 2) cases. Twelve patients required intubation in <24 h, 12 patients in 1–3 days while only three patients were intubated after 3 days. Hence, the requirement of invasive ventilation was clear by the 3rd day of admission in about 89% of patients in whom NIV was failed.
Binary logistic regression
To find out, which variable has a significant effect on the outcome of NIV that is an early predictors of successful NIV treatment, we have applied binary logistic regression for different parameters at admission.
In binary logistic regression, some of the above variables are found to have a significant effect on the outcome of NIV (successful or failure). Considering 0.05 as a significant value of alpha, in our study, we have found that HR, RR, pCO2, pH, and APACHE II score at admission are major predictors of successful NIV management. pO2 and aetiology have no significant value in the prediction.
The optimum cutoff value for APACHE score at admission for predicting the outcome of NIV is 33. Therefore, above 33 scores predict failure of NIV with the following precision.
DISCUSSION
We have conducted the study with 100 randomly selected patients presenting with acute hypercapnic respiratory failure and started on NIV on admission. The study subjects were divided into Group 1 (successful NIV) and Group 2 (failed NIV).
In our study, 73 patients were successfully treated with NIV while 27 required intubation. Therefore, the success rate was 73% in the study. The success rate in various studies is 5–50%. In our study, the age range was 36–75 years and the mean age of patients was 59.6 years. In Group 1, it was 60.24 years and in Group 2, 57.8 years. As COPD is the most common cause, the age distribution was similar to COPD cases. Similar mean values were found in most of the studies where COPD and other causes were included in the study.
In group-wise age distribution, the maximum numbers of patients were in the 50–70 years range. There was no significant effect of age on the success of NIV (P = 0.881). We had 69 males and 31 females in the study. Gender distribution was similar to other studies. There is no significant effect of gender on the success of NIV (n = 0.857).
In our study, COPD was the most common aetiology (80%). Other less common causes were bronchial asthma, neuromuscular disorders, and obstructive sleep apnoea. Aetiology-wise success of NIV is variable in various studies. NIV treatment was successful in 75% of patients with COPD. NIV treatment was successful in 75% of patients with asthma. However, the number of asthma patients was too small (n = 4). Other studies with a greater number of asthma cases have shown variable results with NIV. In a randomised controlled trial, Soroksky et al. have shown that in selected patients with severe asthma, the addition of NIV to conventional treatment can improve lung functions, alleviate exacerbation faster and reduce the need for hospitalisation.[7] The success rate of NIV was about 62% with other aetiologies. In our study, the difference in aetiology did not have a significant effect on the outcome of NIV (P = 0.785). We have also compared the mean days required for different aetiologies.
The sequential improvement in clinical (HR and RR) and ABG (pH, pO2, and pCO2) parameters during treatment on NIV was seen in both groups; however, Group 1 had significantly more improvement as compared to Group 2. HR and RR showed improvement till 1st h of therapy in Group 2, after which they remained almost static. pH worsened from 7.26 to 7.2 after the 1st h. These changes are compared with a paired t-test at each step. As expected, HR and RR show no significant change after 4 h of NIV treatment in Group 2. It indicated that NIV had a positive effect in Group 2 but it was only for the initial few hours and not sufficient to avoid invasive ventilation. Response to NIV may also specify the chances of success. Carratu et al.[8] have shown that patients who improve have increased pH and decreased pCO2 at 2 h pos t-NIV whereas those who fail have no change in these two parameters.
EPAP and IPAP levels in Group 1 decreased from 8.37 to 7.08 and from 14.68 to 14.04, respectively. In Group 2, EPAP and IPAP levels increased from 10.22 to 11.8 and 17.37 to 20.2, respectively. These changes are statistically significant at each step as shown by a paired t-test (0.001).
We have observed the relation of the APACHE II score with the outcome of NIV. Comparison of the APACHE II score at admission and at 24 h shows a significant change in both Groups 1 and 2 (P = 0.001 and 0.007, respectively). However, in Group 1, the change is positive that is, the mean score is decreased from 28 to 23; and in Group 2, it is negative that is, the mean score is increased from 44 to 47. The APACHE II score at admission had a clearly significant effect on the outcome of NIV (P = 0.001) [Figure 6].

- Receiver operating characteristic curve for Acute Physiology and Chronic Health Evaluation II score at admission. Area under the curve=0.965.
We also observed that the greater is the APACHE score; the more are the chances of failure of NIV. It is such that the percentage of failure is 0 when the score is below 30 and 100 when the score is above 50. In various studies, the failure of NIV in uncooperative patients with an APACHE II score of more than 25 has been reported to exceed 50%.[9] In our study, the failure rate with APACHE scores more than 25 was 34% (27 of 79).[10] Bhattacharya states that patients with high APACHE II scores, inability to minimise the amount of mouth leak (because of lack of teeth, secretions, or breathing pattern), or incapacity to synchronise with NIPPV are unlikely to improve with NIPPV and there should be a low threshold for intubation and MV. We did not find any significant effect of aetiology on APACHE score (P = 0.614).
In Group 2 patients, intubation was required in 44% on day 1 of admission, another 44% in the next 2 days, and the remaining 11–12% were intubated after 3 days. Therefore, the failure of NIV is determined in 3 days in most (about 88–89%) of the cases.
Binary logistic regression shows that HR, RR, pH, pCO2, and APACHE II score are the variables significantly affecting the NIV outcome (P < 0.05) [Table 6]. These are the early predictors of the success of NIV in our study. pO2 and aetiology were not significantly affecting the outcome. Hoo et al. did not find significant differences in RR of those who succeeded and those who failed NIV.[11] Wysocki et al. found that those who were successfully ventilated with NIV had a higher pCO2.[12,13] Plant et al., in the prospective multicentre study, found a correlation of APACHE >29 with failure of NIV. Other predictors of early failure were a low pH besides low GCS and also higher APACHE II scores.
| Variable (at admission) | Score | Significance |
|---|---|---|
| HR | 6.536 | 0.011 |
| RR | 29.508 | 0.001 |
| pO2 | 1.099 | 0.294 |
| pCO2 | 7.424 | 0.006 |
| pH | 14.398 | 0.001 |
| APACHE II | 61.738 | 0.001 |
| Aetiology | 1.065 | 0.785 |
HR: Heart rate, RR: Respiratory rate, APACHE II: Acute Physiology and Chronic Health Evaluation II
In the receiver operating characteristic curve plotted for the APACHE II score, the optimum cutoff value was 33 in our study. It gives a sensitivity of 92.6% and a specificity of 86.3%. The area under the curve was 0.965. Various studies have shown cutoff value ranging from 25 to 35.[13] Other predictors of success in our study that is, HR, RR, pCO2, and pH have lesser areas under the curve. The optimum cutoff values for them (132, 353, and 7.18, respectively) are less sensitive and specific as compared to that of the APACHE score.
CONCLUSION
HR,RR,pH,pCO2,APACHE II score at admission are the early predictors of success of NIV in hypercapnic respiratory failure.We can decide on non invasive or invasive ventilation for individual patients with fair precision ,using the cut off values of these indicators.It will help to avoid complications of unindicated invasive ventilation or complications of delayed intubation when it is indicated.
Declaration of patient consent
Consent of Patient/Legally authorised Representative have been taken.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Physiologic effects of positive end-expiratory pressure and mask pressure support during exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1994;149:1069-76.
- [CrossRef] [PubMed] [Google Scholar]
- Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2004;1:CD004104.
- [CrossRef] [Google Scholar]
- Management of COPD exacerbations: A European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017;49:1600791.
- [CrossRef] [PubMed] [Google Scholar]
- Non-invasive positive pressure ventilation in acute respiratory failure due to COPD vs other causes: Effectiveness and predictors of failure in a respiratory ICU in North India. India Int J COPD. 2008;3:737-43.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998-2008. Am J Respir Crit Care Med. 2012;185:152-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative effectiveness of non-invasive and invasive ventilation in critically ill patients with acute exacerbation of chronic obstructive pulmonary disease. Crit Care Med. 2015;43:1386-94.
- [CrossRef] [PubMed] [Google Scholar]
- A pilot prospective, randomized, placebo-controlled trial of bilevel positive airway pressure in acute asthmatic attack. Chest. 2003;123:1018-25.
- [CrossRef] [PubMed] [Google Scholar]
- Early and late failure of non-invasive ventilation in COPD with acute exacerbation. Eur J Clin Invest. 2005;35:4049.
- [CrossRef] [PubMed] [Google Scholar]
- APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818-29.
- [CrossRef] [PubMed] [Google Scholar]
- Recent advances in the role of non-invasive ventilation in acute respiratory failure. Med J Armed Forces India. 2011;67:187-91.
- [CrossRef] [Google Scholar]
- Nasal mechanical ventilation for hypercapnic respiratory failure in chronic obstructive pulmonary disease: Determinants of success and failure. Crit Care Med. 1994;22:1253-61.
- [CrossRef] [PubMed] [Google Scholar]
- Non-invasive pressure support ventilation in patients with acute respiratory failure. Chest. 1993;103:907-13.
- [CrossRef] [PubMed] [Google Scholar]
- Non-invasive ventilation in acute exacerbation of chronic obstructive pulmonary disease: Long term survival and predictors of in-hospital outcome. Thorax. 2001;56:708-12.
- [CrossRef] [PubMed] [Google Scholar]






