Translate this page into:
Innovative Directions in Management of Stable Ischaemic Heart Disease
*Corresponding author: Manish Juneja, Department of Cardiology, Rhythm Heart and Critical Care, Nagpur, Maharashtra, India. drmanishjuneja@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Juneja M, Raut P, Ramteke HD, Walke V, Jolly IT. Innovative Directions in Management of Stable Ischaemic Heart Disease. Vidarbha J Intern Med. doi: 10.25259/VJIM_9_2024
Abstract
The standard approach in the management of coronary artery disease has been based on the postulation that the atherosclerotic plaque, which is causing the obstruction and limiting the flow in the coronary arteries, is the leading cause of angina and myocardial ischaemia in majority of the patients. In the broader perspective, the role of revascularisation therapies have been limited to only patients having left main disease, three vessel diseases along with complications of diabetes or decreased left ventricle ejection fraction. Many studies and new trends showed that extracardiac or non-coronary causes of angina and ischaemia, which include coronary microvascular dysfunction, dysfunctions of myocardial metabolism and vasospastic disorders are neither taken into consideration nor suggested diagnostically. Thus, this creates the urgent need for more innovative approaches and directions for the inclusive management of extracardiac and consideration of revascularisation therapies, which parallelly solves the treatment to the underlying cause and minimizes the risk of angina alongside of ischaemia in the day-to-day clinical practice.
Keywords
Coronary artery disease
Stable ischaemic heart disease
Percutaneous coronary intervention
Coronary artery bypass graft
Myocardial infarction
INTRODUCTION
The science of coronary of angiography is evolving more than half century now. The stable coronary artery disease (CAD) management has been solely based on the significant theory that is supported by anatomic and physiologic evidence. It portrays that flow-limiting atherosclerotic obstructions of the coronary arteries result in cause of angina and myocardial ischaemia in majority of the cardiac cases. This significant theory, which causes the obstruction of coronary arteries or causes severe stenosis, results into acute ischaemia to myocardium or even worse, causing myocardial infarction (MI), which has overwhelmingly influenced in our approach in the management of CAD. In such cases, the revascularisation therapies are used, such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) which can help significantly to restore the blood flow and improve the survival chances to a greater extent.[1] In the major diagnosis, beliefs and many normal considerations still exists that coronary stenosis is the dominant cause of stable angina and leading to ischaemia.[2] The revascularisation therapies have shown significant reduction of high-risk related to CAD, but many clinical trials suggests that revascularisation therapies cannot reduce mortality or morbidity, especially the use of PCI, as compared with guideline directed medical therapy (GDMT).[3-5]
In the acute settings, PCI and CABG revascularising therapies have shown better symptom relief and improved the quality of life (QOL) by 20–30% for angina episode within one year, and 40% within three years,[6,7] which, in the end, leads to repeated PCI or extensive CABG.[8] In the other perspective, repeated angiographies often reveal no evidence of stent restenosis or obstruction, the other preceding factors causing non-obstructive causes of angina must be considered. However, very often in a clinical setting, the cause of angina is more likely to be pushed toward the cause of the obstruction and other pathological factors are not even considered for the diagnostic factors. These pathological factors include microvascular coronary vasospasm, coronary microvascular dysfunction (CMD) and derangements of myocardial energy and varied metabolism.
In a broader sense of view, there is urgent need for a new, more broad, innovative directions and management set for the patients having stable angina, which focuses on the stable angina, obstructive CAD and revascularisation from different perspective and not as a single set. As described many potential pathogenetic mechanisms are responsible for various angina and ischaemia, it is very essential to identify the correct diagnostic and therapeutic approaches for obstructive and non-obstructive causes of myocardial ischaemia. Following these simple steps will lead to more pathogenetic approaches, which would more likely align with proper pharmaceutical therapies and revascularisation therapies in a very synergistic fashion for a various broader population of stable CAD patients.
PERSPECTIVES OF CLINICAL TRIALS
The randomised clinical trial (RCT) has showed that there is no direct benefit in terms of reduction in mortality of the revascularisation therapies, in the case of MI. In fact, in recent years, it was foreseen that many patients with revascularisation therapies like PCI have underwent repeated PCI when added to GDMT.[9] In such situations, multifaceted pharmacologic secondary prevention combined with lifestyle modifications, can lead to significant improvements in health outcomes. However, these results of the trials could not be considered in full percentage. As the studies had various limitations like, subject selection within mild-to-moderate range or having baseline ischaemia, use of bare-metal and use of first generations of stents, various biases were reported like, lack of blinding and Hawthorne effects.[10] These limitations would have led to exclusion of the patients with severe angiographic obstructive disease. A major study named ischaemia, which randomised patients into two categories, from having moderate-to-severe ischaemia, the first category of the patients included initial invasive strategy with revascularisation which included third-generation drug-eluting stent or CABG + GDMT versus GDMT alone.[11,12] It was found that there was no benefit in the invasive approach as the patients would not have any decreased rate of morbidity or mortality. Often in acute conditions, patients would suffer from cardiovascular death; MI resuscitated sudden cardiac death or heart failure. On the long-term conditions, patients would suffer from cardiovascular event-related death. Thus, confirming that there was no improvement in the survival chances, but contrary, there was significant improvement on QOL up to 20% for the onset of angina.[13] A pretrial meta-analysis was done for the clinical trials having GDMT versus GDMT + PCI with stable CAD, where 10 RCTs having 12,125 patients having ischaemia confirmed that PCI did not reduce the mortality rate; furthermore, it explained that GDMT + PCI led to fewer follow-ups and improved anginal symptoms.[14]
Thus, to minimize the potential bias in the unblinded trials, the PCI was studied for the treatment of angina, in a placebo-controlled trial, where two groups, PCI + GDMT versus Placebo procedure + GDMT, was compared showed no incremental improvement in angina relief and physical strenuous activities.[15] Ironically, the study was performed to eliminate the bias, but created controversially numerous amounts of bias, such as small sample size, short follow-up and salutary effect of angina relief.[16] Notably, most of the trials recognised that the management of the patients with stable angina was done due informed and well-considered decision making, whether involving the patient, family or the physician. Thus, both the invasive and conservative approaches were potentially targeted and optimally enhanced the patient-centred outcome.[17]
LIMITATIONS OF REVASCULARISATION THERAPIES
The major limitation that a revascularisation prompt is indicated, that revascularisation has not been shown to reduce the cardiovascular events in the most stable CAD patients.[18] As fundamentally, atherosclerosis is just a systemic vascular and inflammatory condition which affects the coronary and epicardial arteries which affect the microcirculation and other vascular network. Thus, it is very crucial that management of the ischaemia and atherosclerosis must include the lifestyle modification including diet, rest, exercise and cessation of tobacco products. Along the side, there must be intensive risk factor control and multifaceted as a secondary prevention using the pharmacology, having hypertension, dyslipidaemia, diabetes and also followed by inflammation. Thus, having the angina, there must be the effective symptom control.
In a broader perspective, it was observed that the data from the recent large registries have indicated that angina must improve or resolve over time with the proper medical therapy in most of the CAD patients.[19] Thus, the need of revascularisation therapies must be only needed in the very minority of the patients, like 5% in the five-year follow-up schedule.[20] As angina can easily relapse or remit over the time and which results in the coronary plaques, these plaques may remain in arteries and constantly shrinks the outflow; thus, impacting the QOL. In the given situation, three to six months of specific time is required for a complete course of GDMT and efficiently assessed.[21] In other scenarios, the subjects must not be referred for revascularisation just because there is difficulty in achieving the optimal GDMT; particularly, the symptoms are unfrequented or mild. Rather, a very effective GDMT can be achieved by incorporating patients with counselling, targeting a goal toward the patient directed self-care.[22] Some patients who are surely optimal for the GDMT can be treated with lifestyle intervention but some patients having high risk must be taken up for the secondary prevention like revascularisation, but with lack of resources to oversee the intensification of medical therapy lead to cardiovascular event. Hence, more coordinated team management strategies must be fairly used, alongside of the physician extenders and facilitate the optimisation of GDMT and improved patient care. Thus, having standardised patient care pathway and various other management algorithms would improve the chance of proven approaches.
FOCUS ON THE PATHOLOGICAL CAUSE FOR DIAGNOSIS
The most important aspect of the diagnosis during the stable ischaemia heart disease is the view of many causes and its precipitants, along the side of the ischaemia, the SCOT-HEART trial broadly discusses about it.[23] Most of the patients which were known or suspected to have stable CAD, which did not have stenosis having the flow limit indicated that four to five individuals had the underlying cause of angina and ischaemia, which was not directly due to epicardial artery stenosis [Figure 1]. For the underlying reason, complete dependency on the anatomic diagnostic approaches may lead to the invasive coronary angiography (CAG) mat fail to diagnose the microvascular or vasospastic angina, leaving many patients in whom no obstructive coronary lesions are identified and falsely reassured that ischaemia is not present. Often these patients are left confused at which the potential cardiac pathology is not being valued just because the cause is extracardiac leading. In fact, in such cases, there must be more diligent evaluation of non-epicardial coronary causes of angina.
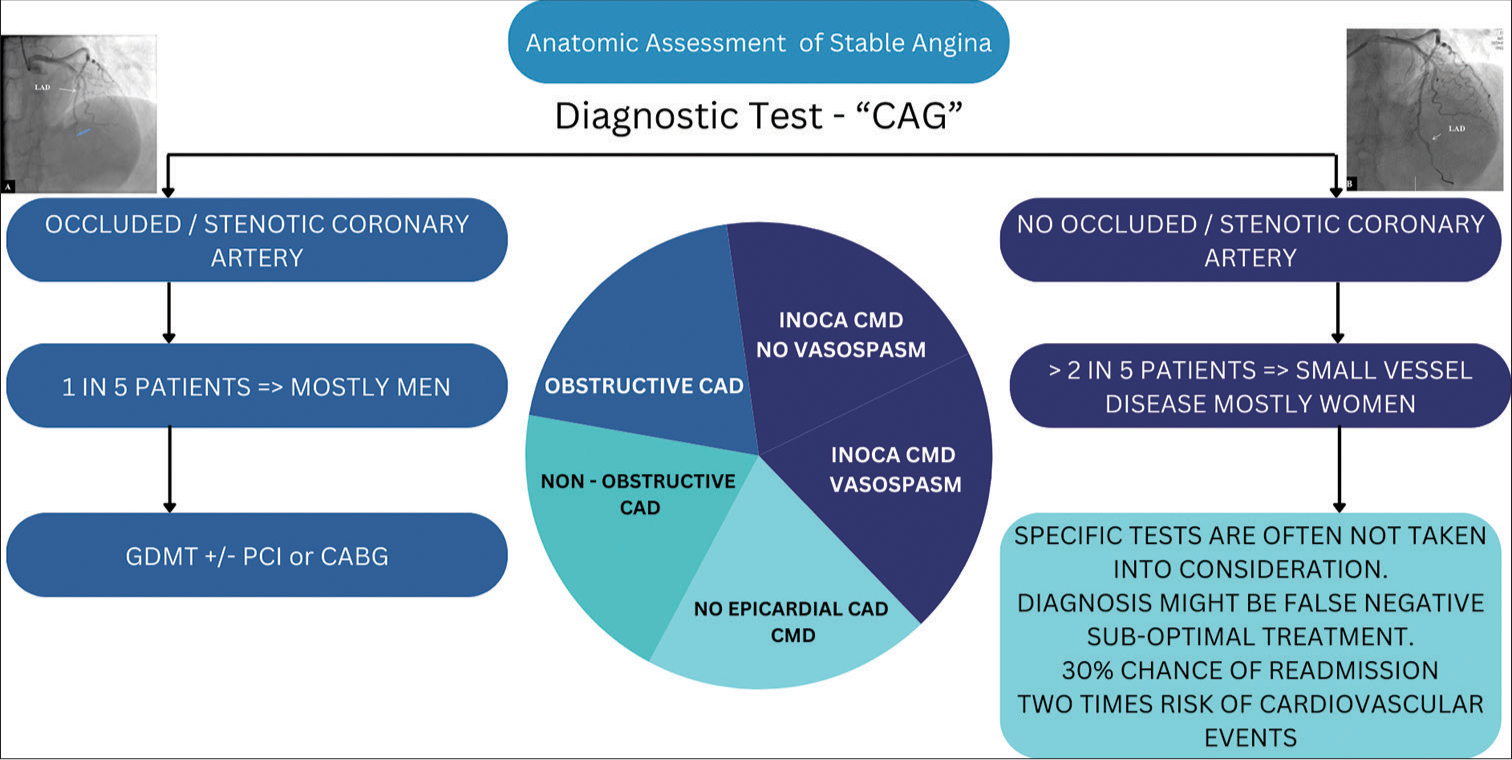
- Clinical pathway of anatomic assessment of stable angina. CAG: coronary angiography, GDMT: guideline directed medical therapy, PCI: percutaneous coronary intervention, CABG: coronary artery bypass grafting, CAD: coronary artery disease, CMD: coronary microvascular dysfunction.
This through investigation must be thoroughly done in the case of women, as most of the patients with ischaemia and having no obstructive coronary arteries (INOCA) are female.[24] Heart disease in women is very under-recognised and undertreated, significantly INOCA, where the failure to account the microvascular and vasospastic angina within the primarily non-invasive anatomic imaging may result in misdiagnosis.[25] Many hospitals have made the CAG as the primary diagnosis test for the angina patients, which may be only helpful in finding the obstructive CAD, which is not even the most common cause of angina and is very less common in women than men.[26]
In a very large observational study, compromising 400,000 angina patients underwent elective CAG found that patients having positive tread mill test, only 41% of them had a very obstructive CAD, which indicated that they need to focus on the various diagnosing factors, like pathophysiologic mechanisms, like CMD and coronary microvascular or epicardial vasospasm. Following the concept of the study, in 2019, the European Society of Cardiology guidelines based on the chronic coronary syndromes stated that among the patients having typical angina, most common range of detecting stable angina was 50–59 years old, out of which 68% of men and 87% of women did not had any of the obstructive coronary stenosis.[27,28] A study of coronary microvascular angina trial and other trials revealed that 45% of the patients presenting with angina or various ischaemia did not have CAD after done with angiography.[29] Including the main aspect, 90% of the patients demonstrated that objective evidence of the coronary and vasomotor dysfunction may be around 81% with CMD. Thus, in the given proportion of suspected stable CAD cases, the CMD or vasoconstriction can also contribute toward the angina, and thus, the mechanisms of this may coexist with the obstructive CAD, the patients having ischaemia may not necessarily or mutually cause the effect of ischaemia.[30] Thus, a complete medical evaluation must be considered for stable angina, including natural history, considering the risk factors and physical examination including pharmacotherapy and treatment. The treadmill test still remains the most useful test to assess the functional capacity and response toward the physiologic stress and limiting symptoms and features of induced ischaemia (mostly symptoms and electrocardiographic changes). The initial plan of management must be based on the antianginal drug therapy, such as short-acting nitrates or beta-blocker along with the calcium channel blocker. This approach balances the need of heart rate of 60 beat/min for CAG.
INNOVATIVE STRATEGIES ACTION PLAN
The American Heart Association and American College of Cardiology chest pain guideline year 2021 along with European Society of Cardiology coronary syndrome guideline year 2019 shows three different mechanisms of stable angina.[31] The first is obstructive CAD, second is coronary vasospasm and the third is CMD. Furthermore, a very basic misinterpretation or misrepresentation is found by not having a standard diagnostic test for patients having suspected angina. Even the anginal chest pain represents the discomfort caused in the heart and often considered as one of the main symptoms of myocardial ischaemia, but it does not provide any specificity in diagnosing the cause. As a result, it is way more far important to diagnose in or diagnose out the obstructive CAD, but also it is used to establish the cause of myocardial ischaemia. This broad diagnostic evaluation not only comprehensively assesses the anatomic but also functional coronary alternations. These alternations help to confirm or exclude the diagnosis of myocardial ischaemia and determine the underlying cause of the myocardial ischaemia or precepting angina.
It has been studied that myocardial perfusion imaging using positron emission tomography (PET) or cardiovascular magnetic resonance imaging (C-MRI) are two most useful tests.[32] This non-invasive imagining technique provides the quantitative and qualitative analysis which is very useful in understanding the underlying cause of ischaemia and angina. Another dynamic first-pass vasodilator stress and rest PET test help in quantifying the absolute myocardial blood flow.[33] The advances with the given stress C-MRI include fully automatic pixel-wise quantitative mapping of myocardial perfusion.[34] In this test, generation of the pixel-encoded maps of myocardial blood flow is calculated in both rest and stress duration. An algorithm for practical assessment of various angina and related ischaemia is proposed in Figure 2. In Figure 2, it illustrates the current international guideline and related studies. The illustration also supports the evidence-based approach of lifestyle interventions and pharmacologic preventions alongside of GDMT. This will try to achieve and maintain various cardiovascular treatment targets for blood pressure, lipid levels and glycaemic levels according to the guidelines of US and Europe.[35,36] The algorithm also found to be significant for anatomic imaging and physiologic explaining in identifying the high risk in the stable CAD patients.
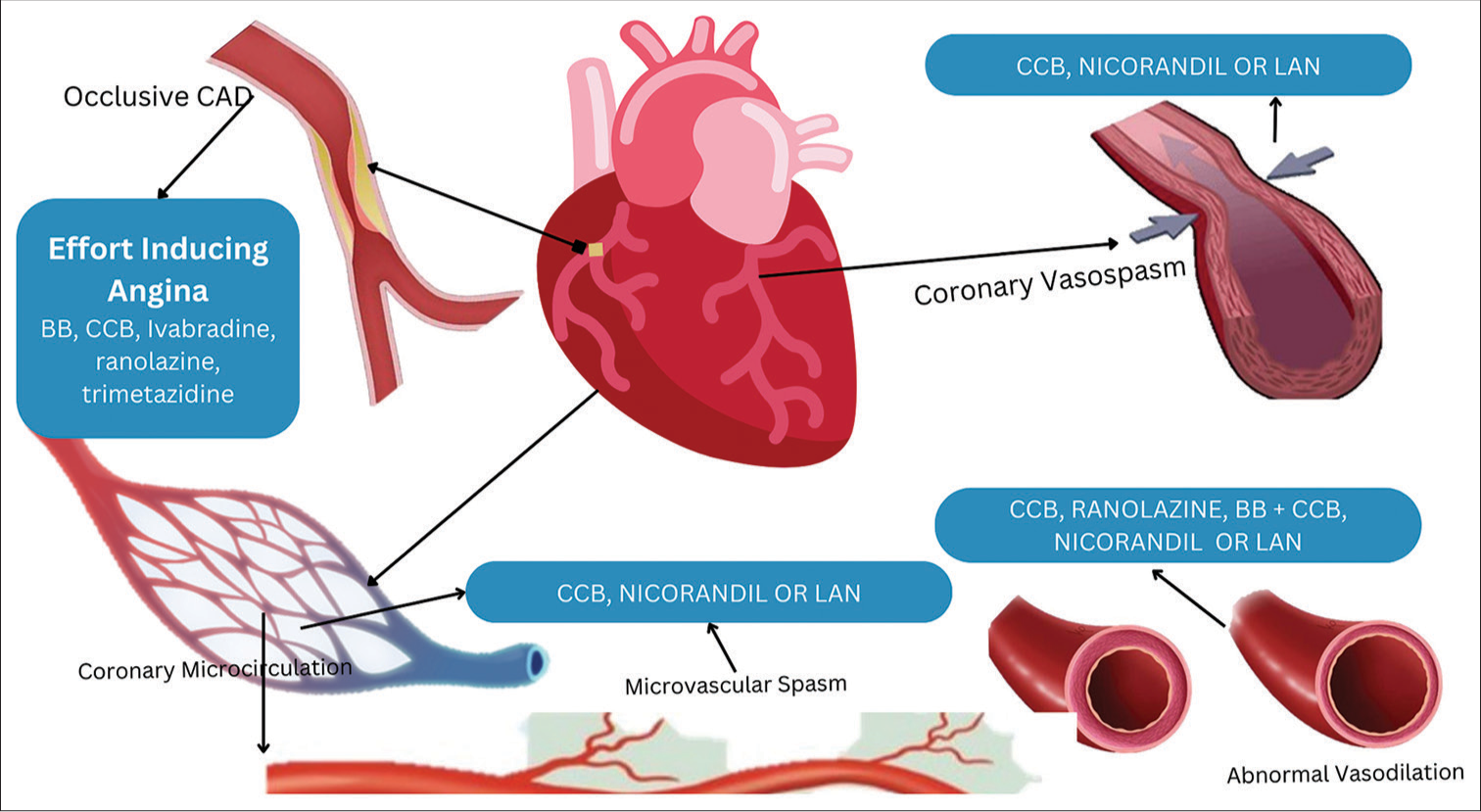
- Clinical pathway of anti-anginal treatment. CAD: coronary artery disease, BB: beta blockers, CCB: calcium channel blockers, LAN: long-acting nitrates.
If non-invasive studies are able to check angina at a very low threshold or a very large ischaemic myocardium which is at the risk for non-invasive stress test, then CAG is most appropriate to exclude or evaluate the CAD-related angina.[18] In all various chronic patients having stable angina, an initial trial of empiric anti-anginal treatment is important for symptom control and various outcomes.[37] Stable CAD patients along with angina must receive the dosage of two antianginal drug classes and must be done for at least 3–6 months before the revascularisation is done.[38]
In patients having persistent or very frequent recurrence of ischaemic symptoms, despite giving the treatment, CAG is indicated to identify the patients for flow-limiting stenoses, followed by revascularisation if needed. In the patients having the obstructive stenosis, the assessment of coronary circulation must be done for acetylcholine to eliminate the spasm, or to maintain the coronary flow reserve and to look for microvascular resistance, and if any of it is shown positive, then patient must be considered for pharmacological treatment.[39] This algorithm allows the physician to look up the clinical situation rather than CAG, which is most widely used in day-to-day clinical practice. In SCOT-HEART trial, it was seen that incidence of non-fatal MI was very low in CAG + PCI-guided group than in the control group, but there was no effect on mortality.[23] It was also found that various drugs such as aspirin and statins consumption were higher in CAG + PCI group rather than the control group. The proposed diagnostic evaluation is proposed in all the stable angina patients for which the obstructive CAD has been excluded, but from the clinical practice perspective, such testing modalities are not available in many hospitals.[40] Thus, the review advices that the various diagnostic testing must and must be done only if the symptoms do not improve or if the obstructive CAD has been excluded from the algorithm.
REASONS FOR INNOVATIVE ACTION PLAN
Physicians must reevaluate their approach and perspective toward the clinical practice of angina-related patients in the given points. First, angina may be due to the complication of obstructive CAD or INOCA. Second, the majority of patients with chronic angina do not exhibit epicardial coronary obstructions; third, if CAG serves as the initial diagnostic test and excludes obstructive coronary stenoses, subsequent testing should involve stress perfusion imaging, PET and/or invasive functional CAG with pharmacologic testing to identify coronary microvascular or vasospastic mechanisms that may necessitate more tailored therapy and, fourth, most INOCA patients are women, and a diagnostic approach solely centred on defining epicardial coronary obstructions might be insufficient.
Interestingly, a comprehensive non-invasive diagnostic approach that considers both anatomical and functional aspects can be achieved through multimodality imaging such as PET/CAG or ‘dynamic’ CAG, offering a non-invasive ‘one-stop shop’ model for diagnosing angina and suspected CAD, encompassing both obstructive and nonobstructive cases. Ongoing randomised controlled trials will determine whether dynamic CAG can deliver on this potential.
THERAPEUTIC MANAGEMENT FOR ANGINA AND ISCHAEMIA
A decrease in coronary/myocardial flow reserve may indicate ischaemia resulting from epicardial stenoses, impaired microvascular function or both, even within the same patient, as previously mentioned. In such cases, medications that lower myocardial oxygen consumption such as beta-blockers, no dihydropyridine calcium-channel blockers or ivabradine or improve myocardial oxygen utilisation such as ranolazine or trimetazidine are likely the most suitable options. Combining these medications can also be considered [Figure 3]. Alternatively, ischaemia can also be triggered by epicardial or microvascular spasms. In such instances, vasodilators such as calcium-channel blockers, nitrates or nicorandil are the most appropriate choice, and combining them can also be considered. Therefore, it is highly desirable, whenever possible, to tailor pharmacological therapies to the underlying causes and triggers of ischaemia.
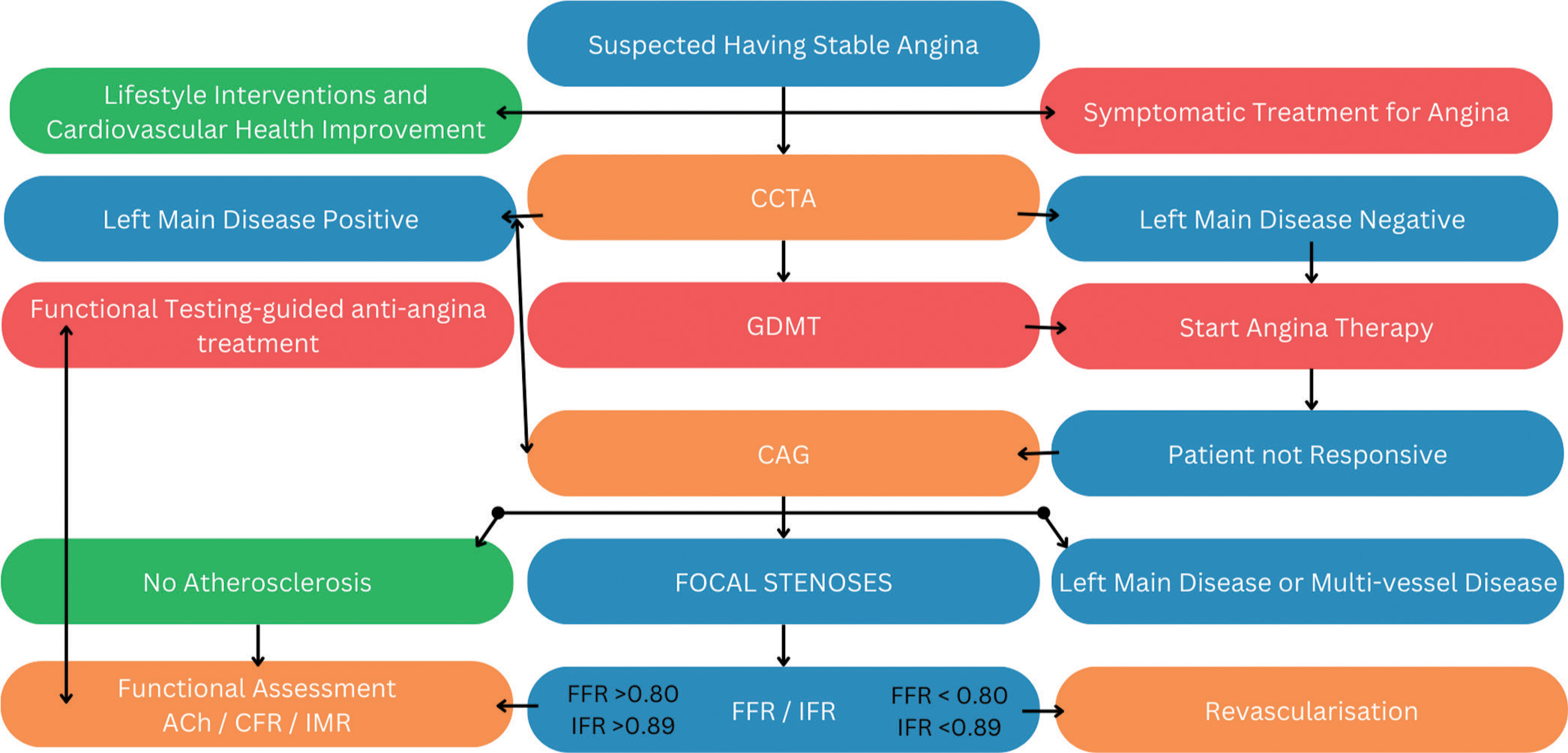
- Algorithm for innovative directions in management of stable ischaemic heart disease. ACh: acetylcholine, CFR: coronary flow reserve, IMR: index of microvascular resistance, FFR: fractional flow reserve, IFR: instantaneous wave-free ratio, CAG: coronary angiography, GDMT: guideline directed medical therapy, CCTA: coronary computed tomography angiography.
CONCLUSION
It is time to rethink how we manage stable CAD patients. First, we need to broaden our understanding of the various causes and mechanisms behind angina and myocardial ischaemia, moving away from solely associating ischaemia with obstructive epicardial disease. Angina and ischaemia can stem from multiple causes, not solely epicardial coronary obstruction. Therefore, our terminology should reflect this broader understanding, perhaps using terms like ‘acute and chronic myocardial ischaemic syndromes’. Second, we should adopt a more holistic management approach. Ischaemia assessments without abnormal coronary angiographic findings should prompt consideration of no epicardial coronary causes, such as CMD and vasospastic disorders, rather than immediately attributing symptoms to non-cardiac issues. Treatment plans for angina and ischaemia must be personalised for each patient, although implementing available diagnostic tools for personalised approaches in clinical practice remains challenging. Third, we need to invest in developing new management strategies and health-care delivery models aligned with treatments proven to benefit patients and society. Despite established clinical practice guidelines, proven secondary prevention strategies and lifestyle interventions are underutilised, especially in the United States. Integrating preventive therapies alongside procedural and pharmacologic interventions can enhance event-free survival and improve outcomes in stable CAD patients, emphasising the complementary nature of these approaches in achieving optimal clinical outcomes and symptom relief.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that they have used artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript or image creations.
Financial support and sponsorship
Nil.
References
- Updates in the Management of Coronary Artery Disease: A Review Article. Cureus. 2023;15:e50644.
- [CrossRef] [Google Scholar]
- Angina in 2022: Current Perspectives. J Clin Med. 2022;11:6891.
- [CrossRef] [PubMed] [Google Scholar]
- 2021 ACC/AHA/SCAI Guideline for Coronary Artery Revascularization: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e18-114.
- [CrossRef] [Google Scholar]
- Revascularization Strategies for Patients with Stable Coronary Artery Disease. J Intern Med. 2014;276:336-51.
- [CrossRef] [PubMed] [Google Scholar]
- Recent Advances in Coronary Artery Bypass Grafting Techniques and Outcomes: A Narrative Review. Cureus. 2023;15:e45511.
- [CrossRef] [Google Scholar]
- Meta-analysis of 5-year Outcomes of CABG vs PCI with Stenting in Patients with Multivessel Disease. Minerva Cardioangiol. 2008;56:453-60.
- [Google Scholar]
- Five-Year Outcomes after PCI or CABG for Left Main Coronary Disease. N Engl J Med. 2019;381:1820-30.
- [CrossRef] [PubMed] [Google Scholar]
- Percutaneous Coronary Intervention with Stenting versus Coronary Artery Bypass Grafting in Stable Coronary Artery Disease. Int J Angiol. 2021;30:221-7.
- [CrossRef] [PubMed] [Google Scholar]
- Five-year Outcomes after State-of-the-art Percutaneous Coronary Revascularization in Patients with De novo Three-vessel Disease: Final Results of the SYNTAX II Study. Eur Heart J. 2022;43:1307-16.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing CABG and PCI Across the Globe based on Current Regional Registry Evidence. Sci Rep. 2022;12:22164.
- [CrossRef] [PubMed] [Google Scholar]
- ISCHEMIA Trial: Was It Worth the Wait? Circulation. 2020;142:517-9.
- [CrossRef] [PubMed] [Google Scholar]
- An Initial Strategy of Intensive Medical Therapy is Comparable to that of Coronary Revascularization for Suppression of Scintigraphic Ischemia in High-risk but Stable Survivors of Acute Myocardial Infarction. J Am Coll Cardiol. 2006;48:2458-67.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of PCI on Long-Term Survival in Patients with Stable Ischemic Heart Disease. N Engl J Med. 2015;373:1937-46.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Optimizing Guideline-Directed Medical Therapy Before Discharge on Mortality and Heart Failure Readmission in Patients Hospitalized With Heart Failure With Reduced Ejection Fraction. Am J Cardiol. 2018;121:969-74.
- [CrossRef] [PubMed] [Google Scholar]
- A Placebo-Controlled Trial of Percutaneous Coronary Intervention for Stable Angina. N Engl J Med. 2023;389:2319-30.
- [CrossRef] [PubMed] [Google Scholar]
- Bias and Loss to Follow-Up in Cardiovascular Randomized Trials: A Systematic Review. J Am Heart Assoc. 2020;9:e015361.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and Management of Stable Angina: A Review. JAMA. 2021;325:1765-78.
- [CrossRef] [PubMed] [Google Scholar]
- Routine Revascularization Versus Initial Medical Therapy for Stable Ischemic Heart Disease: A Systematic Review and Meta-Analysis of Randomized Trials. Circulation. 2020;142:841-57.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary Computed Tomography Angiography Compared With Single Photon Emission Computed Tomography Myocardial Perfusion Imaging as a Guide to Optimal Medical Therapy in Patients Presenting With Stable Angina: The RESCUE Trial. J Am Heart Assoc. 2020;9:e017993.
- [CrossRef] [PubMed] [Google Scholar]
- The Long-Awaited Revascularization Guidelines Are Out: What's In Them? Circulation. 2022;145:155-7.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of Life after PCI with Drug-eluting Stents or Coronary-artery Bypass Surgery. N Engl J Med. 2011;364:1016-26.
- [CrossRef] [PubMed] [Google Scholar]
- Myocardial Revascularization in Patients with Ischemic Cardiomyopathy: For Whom and How. J Am Heart Assoc. 2023;12:e026943.
- [CrossRef] [PubMed] [Google Scholar]
- Low-Attenuation Noncalcified Plaque on Coronary Computed Tomography Angiography Predicts Myocardial Infarction: Results From the Multicenter SCOT-HEART Trial (Scottish Computed Tomography of the HEART) Circulation. 2020;141:1452-62.
- [CrossRef] [PubMed] [Google Scholar]
- Ischemia with No Obstructive Arteries (INOCA): A Review of the Prevalence, Diagnosis and Management. Curr Probl Cardiol. 2023;48:101420.
- [CrossRef] [PubMed] [Google Scholar]
- Heart Disease in Women: A Narrative Review. Anaesthesia. 2021;76(Suppl 4):118-30.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation and Management of Patients With Stable Angina: Beyond the Ischemia Paradigm: JACC State-ofthe-Art Review. J Am Coll Cardiol. 2020;76:2252-66.
- [CrossRef] [PubMed] [Google Scholar]
- 2019 ESC Guidelines for the Diagnosis and Management of Chronic Coronary Syndromes. Eur Heart J. 2020;41:407-77.
- [CrossRef] [PubMed] [Google Scholar]
- Beta Blockers, Calcium Channel Blockers, and Long-acting Nitrates for Patients with Stable Angina and Low Blood Pressure Levels: Should This Recommendation Be Reconsidered? Eur Heart J. 2020;41:479.
- [CrossRef] [PubMed] [Google Scholar]
- Rationale and Design of the British Heart Foundation (BHF) Coronary Microvascular Angina (CorMicA) Stratified Medicine Clinical Trial. Am Heart J. 2018;201:86-94.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary Microvascular Dysfunction: A Review of Recent Progress and Clinical Implications. Front Cardiovasc Med. 2023;10:1111721.
- [CrossRef] [PubMed] [Google Scholar]
- 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021;144:e368-454. Erratum in: Circulation 2021;144:e455. Erratum in: Circulation 2023;148:e281
- [CrossRef] [Google Scholar]
- Diagnostic Accuracy of Stress Myocardial Perfusion Imaging Compared to Invasive Coronary Angiography with Fractional Flow Reserve Meta-analysis. Circ Cardiovasc Imaging. 2015;8:e002666.
- [CrossRef] [PubMed] [Google Scholar]
- Noninvasive Assessment of Myocardial Perfusion. Circ Cardiovasc Imaging. 2009;2:412-24.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic Performance of Fully Automated Pixel-Wise Quantitative Myocardial Perfusion Imaging by Cardiovascular Magnetic Resonance. JACC Cardiovasc Imaging. 2018;11:697-707.
- [CrossRef] [PubMed] [Google Scholar]
- Target Blood Pressure for Treatment: Should Current Recommendations Be Changed? Hypertension. 2016;68:263-5.
- [CrossRef] [PubMed] [Google Scholar]
- Guideline-Driven Management of Hypertension: An Evidence-Based Update. Circ Res. 2021;128:827-46.
- [CrossRef] [PubMed] [Google Scholar]
- Recent Advances in the Management of Chronic Stable Angina II. Anti-Ischemic Therapy, Options for Refractory Angina, Risk Factor Reduction, and Revascularization. Vasc Health Risk Manag. 2010;6:749-74.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Chronic Stable Angina. Crit Care Nurs Clin North Am. 2017;29:487-93.
- [CrossRef] [PubMed] [Google Scholar]
- Invasive Assessment of the Coronary Microvasculature: The Index of Microcirculatory Resistance. Circ Cardiovasc Interv. 2017;10:e005361.
- [CrossRef] [PubMed] [Google Scholar]
- Predicting the Benefits of Percutaneous Coronary Intervention on 1-Year Angina and Quality of Life in Stable Ischemic Heart Disease: Risk Models From the COURAGE Trial (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) Circ Cardiovasc Qual Outcomes. 2018;11:e003971.
- [CrossRef] [PubMed] [Google Scholar]






