Translate this page into:
Opaque Hemithorax in a Young Girl: A Rare Case of Askin’s Tumour
*Corresponding author: Gyanshankar Mishra, Department of Respiratory Medicine, Indira Gandhi Government Medical College, Nagpur, Maharashtra, India. gpmishra81@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Wankhede D, Munje R, Mishra G, Gaur S. Opaque Hemithorax in a Young Girl: A Rare Case of Askin’s Tumour. Vidarbha J Intern Med. doi: 10.25259/VJIM_13_2024
Abstract
Askin’s tumor is a primitive neuroectodermal tumor primarily affecting the thoracopulmonary region. It typically manifests in children and adolescents, with a notable female preponderance. Histologically, it presents as a malignant small blue cell tumor. Clinical presentation often includes respiratory symptoms such as pain, dyspnoea, and weight loss. Prognosis is generally unfavorable with a median survival of around 8 months and an overall survival rate of approximately 60% at 5 years. This report highlights the case of a 13-year-old female diagnosed with Askin’s tumor. This report highlights the case of a 13-year-old female presented with a 2-month history of back pain, right-sided chest pain, exertional breathlessness, and loss of appetite. Examination revealed dyspnoea, pallor, and bilateral cervical lymphadenopathy. Radiological and histopathological investigations confirmed the diagnosis of Askin’s tumor with malignant pleural effusion and distant metastasis. This case underscores the importance of considering Askin’s tumor in the differential diagnosis of thoracic masses in pediatric patients. Early recognition and a multidisciplinary approach are crucial for optimizing patient outcomes.
Keywords
Unilateral opaque hemithorax
Askin’s tumour
Blue cell tumour
Paediatric malignancy
INTRODUCTION
The term “white hemithorax” or “opaque hemithorax” refers to a radiopaque hemithorax observed on chest radiography. This radiopacity is typically homogeneous in density but may occasionally include scattered areas of air or calcium. A white hemithorax is a common finding on paediatric chest radiographs and can be attributed to various chest disorders.
Clinical details, including the patient’s age, symptoms and the position of mediastinal structures, are crucial for accurate differential diagnosis and correct identification of the underlying condition.[1]
The aetiology of certain conditions can often be inferred from the mediastinal position. In paediatric cases where the mediastinum shifts towards the ipsilateral side, potential causes include total lung collapse due to a large foreign body, pulmonary agenesis or pulmonary hypoplasia. Conversely, if there is no mediastinal shift, possible causes include consolidation, pulmonary oedema/ acute respiratory distress syndrome and pleural or chest wall masses such as mesothelioma or Askin’s/Ewing sarcoma. When the mediastinum is displaced towards the contralateral side, potential aetiologies include pleural effusion, diaphragmatic hernia, large pulmonary masses or diaphragmatic rupture. Recognising these positional changes in the mediastinum aids in the diagnostic process, guiding clinicians towards appropriate investigations and management strategies.[1]
Ewing sarcoma, peripheral primitive neuroectodermal tumours and Askin’s tumours are categorised under the “Ewing family of tumours,” characterised by varying degrees of neuroectodermal differentiation. Histologically, these tumours exhibit small round blue cells.[2]
Askin’s tumour is a rare neoplasm of the thoracopulmonary region. However, it often mimics other common paediatric disorders such as empyema, lymphoma and tuberculosis, posing significant diagnostic and therapeutic challenges. Early diagnosis and appropriate referral/treatment are crucial in such cases. Due to its rarity, established treatment guidelines for Askin’s tumours are lacking. Most treatment centres adopt a multimodal approach involving chemotherapy, surgery and radiotherapy to manage this aggressive malignancy. Further research is warranted to refine therapeutic strategies and improve outcomes for patients with Askin’s tumours.[3]
CASE REPORT
We present the case of a 13-year-old female who presented with a two-month history of back pain and right-sided chest pain, accompanied by exertional breathlessness and loss of appetite for the past eight days. There was no history of trauma.
Clinical examination
On examination, the patient appeared dyspnoeic and exhibited pallor and bilateral cervical lymphadenopathy. She did not show signs of icterus, cyanosis, clubbing or oedema. Respiratory system inspection revealed a positive trail sign on the left side, fullness of the intercostal space on the right side, decreased movement on the right side and an unvisualised apical impulse. Palpation indicated tracheal deviation to the left. Percussion demonstrated a stony dull note without shifting dullness on the right hemithorax. Auscultation revealed absent breath sounds on the right hemithorax, while the left side was normal. These findings were suggestive of a gross right-sided pleural effusion. The rest of the systemic examination was unremarkable.
Radiological and imaging findings
Chest radiograph (January 25, 2024)
The chest X-ray showed a right-sided opaque hemithorax with a mediastinal shift to the opposite side [Figure 1].

- Chest X-ray (PA view) showing right-sided homogeneous opacity with mediastinal shift to the left.
Ultrasonography (January 26, 2024)
Ultrasonography of the thorax indicated gross free fluid in the right pleural space with maximum interpleural separation of 8 cm and pleural thickening up to 10.8 cm. There was underlying collapsed/consolidated lung parenchyma on the right side and minimal free fluid in the left pleural space. Ultrasonography of the abdomen suggested intra-abdominal lymphadenopathy [Figure 2].
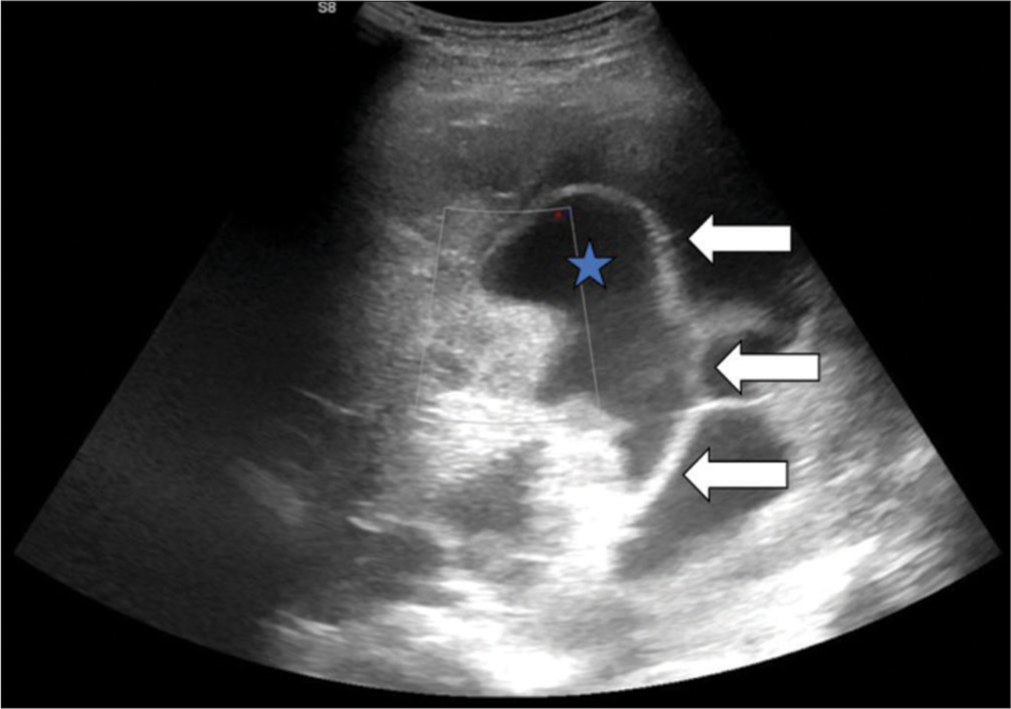
- Ultrasonography of the thorax showing pleural fluid (blue star) with multiple septa (white arrows).
Contrast-enhanced computed tomography (CECT) (June 27, 2024)
The CECT scan of the thorax revealed nodular and thickened right pleura, a gross pleural collection with underlying lung parenchyma collapse/consolidation and suspicious invasion into the deep muscular plane of the anterolateral and posterior chest wall on the right side. In addition, there was focal sclerosis and cortical erosion along the posterior aspect of the 5th rib on the right side, with multiple subcentimetre to enlarged heterogeneously enhancing lymph nodes in various regions, suggesting metastasis. The differential diagnoses included Askin’s tumour, tuberculosis and lymphoma [Figure 3].
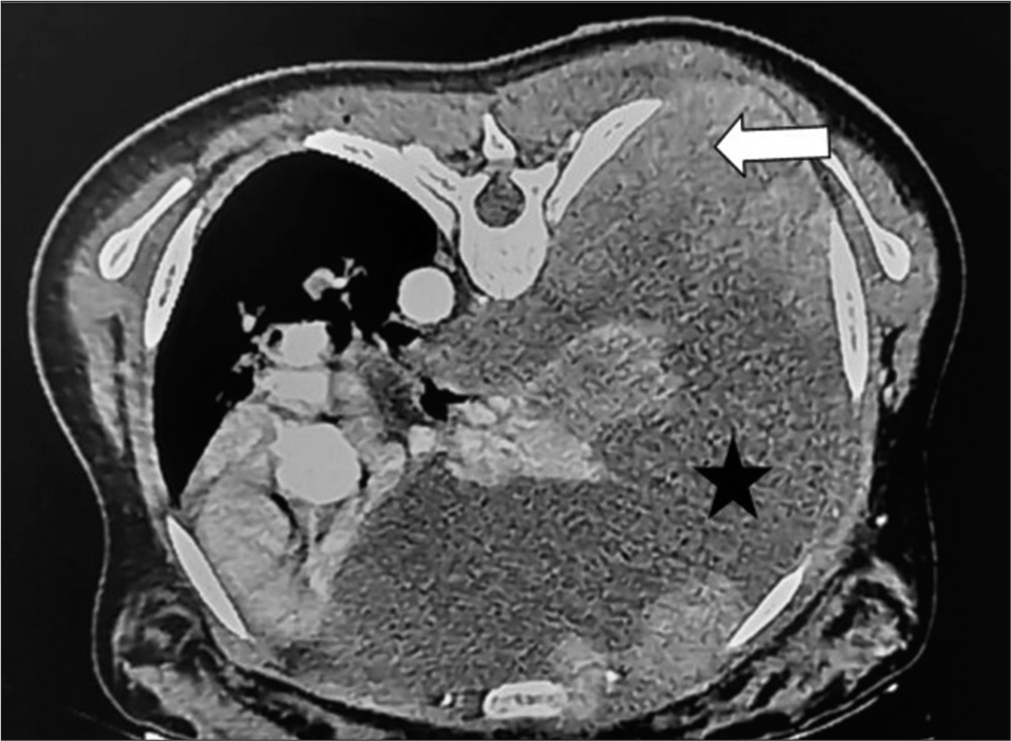
- Contrast-enhanced computed tomography thorax showing nodular and thickened right pleura (white arrow) with a gross right pleural collection (star shaped).
Magnetic resonance imaging (MRI) (February 01, 2024)
The MRI of the thorax showed diffuse circumferential nodular pleural thickening on the right side, involving the posterior thoracic wall and extending into the spinal canal, consistent with a malignant neoplastic aetiology. There were a few enlarged altered signal intensity lesions in the right para-aortic region, possibly indicating metastasis. Mild ascites were also noted [Figure 4].
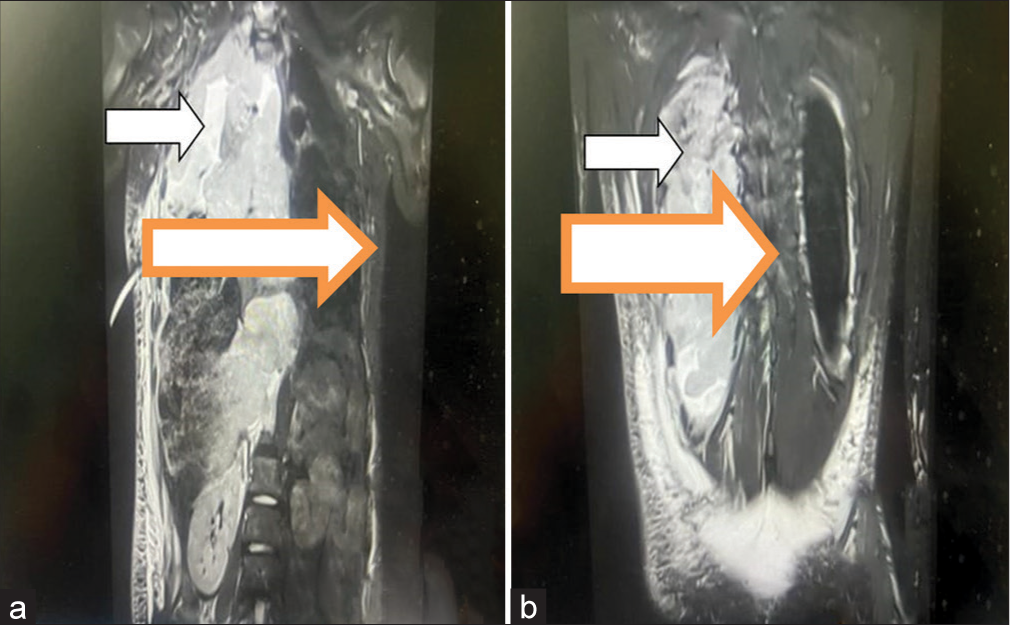
- (a and b) Magnetic resonance imaging scan of the thorax (sagittal section): pleural thickening (white arrow), Intercostal drainage tube seen in situ in 5th intercostal space with its tip towards the apical segment of the right upper lobe (4a).
Histopathology (January 29, 2024)
The lung biopsy was suggestive of a malignant small round blue cell tumour [Figure 5].
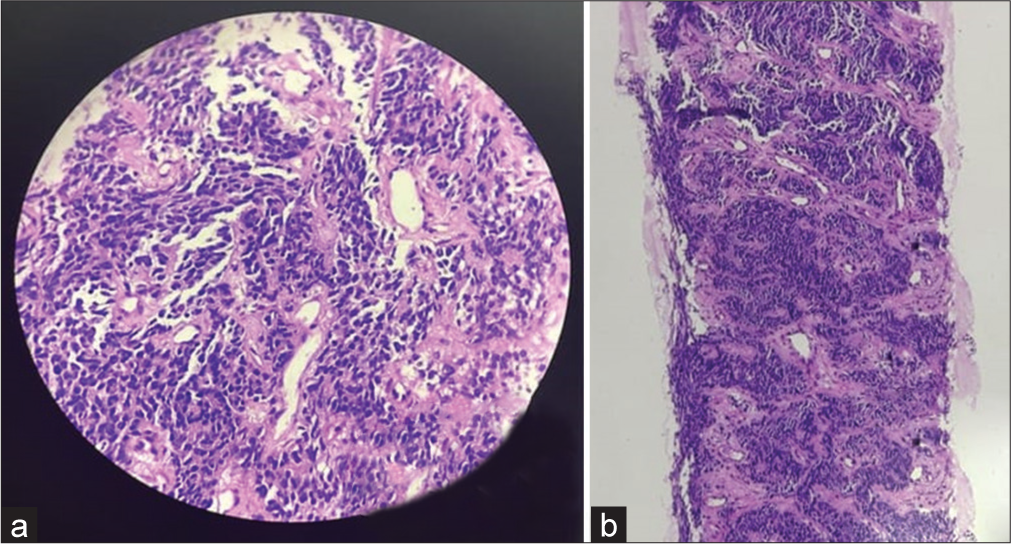
- (a and b) Histopathology showing malignant small round blue cells.
Pleural fluid analysis
The pleural fluid analysis indicated an exudative fluid with low adenosine deaminase [Table 1].
| Colour | Pale yellow |
|---|---|
| Transparency | Slightly hazy |
| Adenosine deaminase (ADA) | 14.7U/L |
| Protein | 3.68 gm/dl |
| Glucose | 63 mg/dl |
| Total leucocyte count | 1300 cells/cumm |
| Differential leucocyte count | “Lymphocyte -90% Polymorph – 10%” |
| Acid Fast Bacilli | Negative |
| Carcinoembryonic Antigen (CEA) | 0.50 ng/ml |
Immunohistochemistry (IHC)
IHC of the lung biopsy specimen was suggestive of Ewing sarcoma family of tumours with various markers [Figure 6 and Table 2].
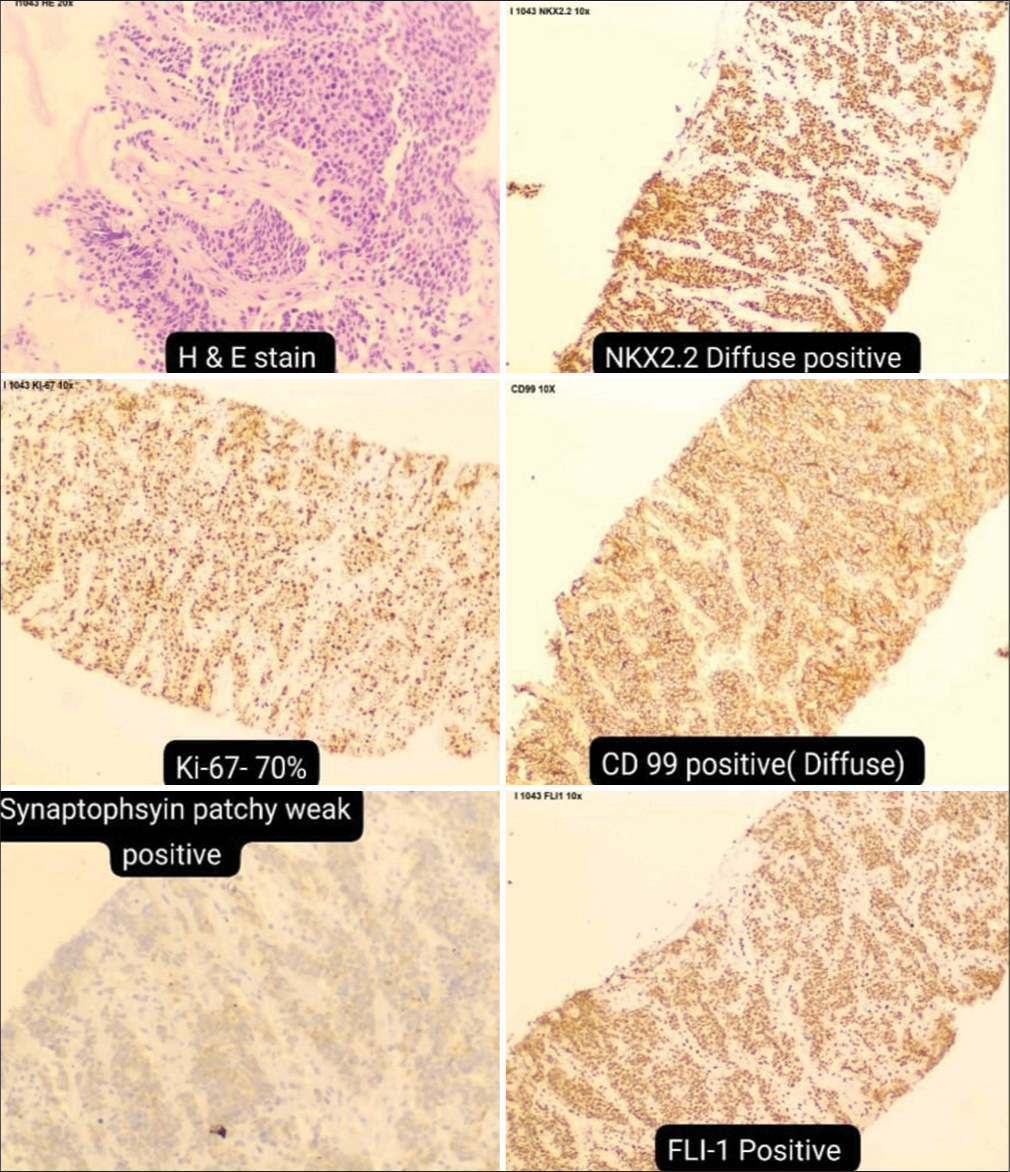
- Immunohistochemistry markers indicating Ewing’s sarcoma. H & E: Hematoxylin and eosin staining, NKX2.2: NK2 homeobox 2, Ki-67: Antigen Kiel 67, CD-99: cluster of differentiation 99, FLI-1: Friend leukemia integration 1.
| IHC Markers | Result |
|---|---|
| NK2 homeobox 2 (NKX2-2) | Diffuse Positive |
| Desmin | Negative |
| Cytokeratin (CK) | Negative |
| Leukocyte Common Antigen (LCA) | Negative |
| Antigen kiel 67 (Ki - 67) | 70% |
| Cluster of Differentiation 99 (CD 99) | Positive (Diffuse) |
| Synaptophysin | Patchy weak positive |
| Friend leukemia integration 1 (FLI1) | Positive |
| Chromogranin A | Negative |
Diagnosis
Following comprehensive assessment and investigations, the final diagnosis was established as Askin’s tumour with malignant pleural effusion and distant metastasis.
DISCUSSION
The present case involved a right-sided thoracic mass accompanied by straw-coloured pleural effusion. The differential diagnosis included malignant lesions such as lymphoma, Ewing sarcoma, neuroblastoma, rhabdomyosarcoma and primitive neuroectodermal tumour. The rarity of Askin’s tumour, along with its clinical presentation, imaging findings and outcomes, has been documented in only a few case reports from India. Poor prognostic indicators for Askin’s tumour include age over 18 years, poor response to induction chemotherapy and the presence of pleural effusion.[3]
Askin’s tumour, a rare neoplasm predominantly affecting the thoracopulmonary region, demonstrates a proclivity for the soft tissues of the chest wall, rib periosteum, chest and lung. Although it can manifest at any age, it predominantly occurs in children and young adults, with a heightened occurrence among individuals of Caucasian descent. Clinical presentation often encompasses a painful chest wall mass accompanied by symptoms such as dyspnoea, cough, weight loss, Horner’s syndrome or regional lymphadenopathy. Radiographically, a chest wall soft-tissue density mass, potentially associated with rib erosion and/or pleural effusion, is commonly observed.[4]
For diagnostic confirmation and staging of Askin’s tumour, the current recommendations advocate for the utilisation of thoracoscopy and positron emission tomography-CT scan. These modalities offer indispensable insights into the extent of tumour involvement and intrathoracic extension, thereby facilitating precision in treatment planning. In addition, IHC assumes a pivotal role in tailoring chemotherapy regimens, thereby enabling a personalised therapeutic approach. Despite aggressive therapeutic interventions comprising chemotherapy and radiotherapy, the overall 5-year survival rate stands at approximately 60%. Notably, MRI features of Askin’s tumours typically manifest as heterogeneous soft-tissue masses exhibiting moderate-to-high signal intensity on T1-weighted images, surpassing that of skeletal muscle and high signal intensity on T2-weighted images. The utilisation of MRI aids in further characterisation of the tumour and evaluation of its spatial relationship with adjacent anatomical structures.[5]
Therefore, Askin’s tumour poses a formidable challenge, mandating a multidisciplinary strategy for precise diagnosis, staging and treatment formulation. Timely identification and intervention hold paramount importance in maximising patient outcomes in this rare yet clinically impactful pathology.[6]
CONCLUSION
In summary, Askin’s tumour represents a rare neoplasm primarily localised in the thoracopulmonary region. However, its clinical presentation often mimics other common paediatric disorders such as empyema, lymphoma and tuberculosis, thus presenting a significant diagnostic and therapeutic challenge to clinicians. Hence, early diagnosis and appropriate referral/treatment are imperative in such cases.
Pleural effusions can serve as a presenting sign of malignancy in the paediatric population, warranting active diagnostic workup.
The Ewing family of tumours, known for their aggressive nature, may lead to late presentations with symptoms indicative of metastasis (e.g., backache) alongside primary symptoms like breathlessness. Therefore, a proactive approach to diagnosis and treatment is essential in such scenarios.
Considering Askin’s tumour within the spectrum of thoracic neoplasms is crucial. On confirmation of a primitive neuroectodermal tumour diagnosis, optimal management involves a multimodal approach, incorporating neoadjuvant chemotherapy alongside surgical resection and/or postoperative radiotherapy. This comprehensive strategy aims to minimise local recurrence and prolong disease-free intervals. Given its aggressive behaviour, strict adherence to follow-up protocols is paramount for monitoring these patients effectively.
Ethical approval
Institutional review board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Unilateral Lung Whiteout in Children: Four Cases and a Discussion of Management. Pediatr Emerg Care. 2019;35:e1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Askin Tumor: A Rare Neoplasm of Thoracopulmonary Region. Lung India. 2016;33:196-8.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant Small Cell Tumor of the Thoracopulmonary Region in Childhood: A Distinctive Clinicopathologic Entity of Uncertain Histogenesis. Cancer. 1979;43:2438-51.
- [CrossRef] [PubMed] [Google Scholar]
- Biology and Treatment of Thoracic Tumors of Neural Crest Origin Thoracic Oncology Philadelphia, PA: Saunders; 1989. p. :520-40.
- [Google Scholar]
- Askin's Tumor: A Case Report and Literature Review. World J Surg Oncol. 2013;11:10.
- [CrossRef] [PubMed] [Google Scholar]






