Translate this page into:
A Study of NT-ProBNP and ETCO2 in Patients Presenting with Acute Dyspnoea
*Corresponding author: Dr. Riya Saboo, Department of General Medicine, Government Medical College and Hospital, Nagpur, Maharashtra, India. riya.saboo26@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Saboo R, Chand D. A Study of NT-ProBNP and ETCO2 in Patients Presenting with Acute Dyspnoea. Vidarbha J Intern Med 2022;32:94-9.
Abstract
Objectives:
In patients presenting with acute dyspnoea in the emergency department (ED), the early and correct diagnosis may present a significant clinical challenge. The most common diagnoses of acute shortness of breath and manifesting signs of respiratory distress are decompensated heart failure (HF), pneumonia, chronic obstructive pulmonary disease (COPD), pulmonary embolism (PE), asthma, and acute respiratory distress syndrome (ARDS) and other causes like anaemia. The aim of the study was to measure NT-pro brain natriuretic peptide (BNP) and exhaled end-tidal carbon dioxide (ETCO2) in patients presenting with dyspnoea.
Material and Methods:
This prospective, cross-sectional and observational study was performed at the Government Medical College and Hospital, Nagpur, between October 2019 and October 2021 in patients admitted to the medicine intensive care unit. Three groups of patients were compared: (1) HF-related acute dyspnoea group (n = 52), (2) pulmonary (COPD/PE)-related acute dyspnoea group (n = 31) and (3) sepsis with ARDS-related dyspnoea group (n = 13). All patients underwent initial clinical examination with a recording of initial vital parameters along with on-admission ETCO2 measurement, NT-proBNP testing, arterial blood gas testing, lung ultrasound examination, 2D echocardiography, chest X-rays, and other basic diagnostic laboratory testing.
Results:
We included 96 patients during the study period. Median NT-proBNP was found to be maximum for the HF group (11,480 pg/ml) followed by the sepsis group (780 pg/ml) and pulmonary group (231 pg/ml). The mean ETCO2 value was found to be maximum in the pulmonary group (48.610 mmHg) followed by HF (31.51 mmHg) and the sepsis group (19.46 mmHg). All results were found to be statistically significant (P < 0.05).
Conclusion:
NT-proBNP has high diagnostic accuracy in differentiating acute HF-related dyspnoea from pulmonary (COPD and ARDS)-related acute dyspnoea. The higher levels of ETCO2 help in diagnosing patients with COPD.
Keywords
NT-pro brain natriuretic peptide (NT-Pro BNP)
Exhaled end-tidal carbon dioxide (ETCO2)
Dyspnoea
INTRODUCTION
Dyspnoea, commonly referred to as shortness of breath, is the subjective sensation of uncomfortable breathing composed of qualitatively distinct sensations that vary in intensity. In patients presenting with acute dyspnoea in a pre-hospital setting, the early and correct diagnosis may present a significant clinical challenge. Epidemiologically, the most common diagnoses among adult patients presenting to an emergency department (ED) with a complaint of acute shortness of breath and manifesting signs of respiratory distress are decompensated heart failure (HF), pneumonia, chronic obstructive pulmonary disease (COPD), pulmonary embolism (PE), asthma, acute respiratory distress syndrome (ARDS) and other causes like anaemia. Differentiating between dyspnoea due to cardiac cause and obstructive airway disease is an important aspect of patient assessment in the ED.[1] It can be differentiated based on various parameters such as clinical history, presentation of the patient, biomarkers, and imaging studies to help appropriately targeted therapy.[2] The pre-hospital settings are unlikely to have such diagnostic tests available, so a fast, non-invasive tool is needed to objectively differentiate between these two common causes of dyspnoea. This can be achieved with the use of exhaled end-tidal carbon dioxide (ETCO2), a continuous variable that is determined by basal metabolic rate, cardiac output, and ventilation, this can be measured non-invasively by capnography providing valuable information for assessment of the cause of dyspnoea. Obstructive pulmonary disease (COPD/asthma) is characterised in part by hypoventilation, retention of carbon dioxide, and high PaCO2, while pulmonary oedema caused by congestive HF (CHF) is characterised by poor alveolar oxygen exchange and increased ventilation with ETCO2 levels being significantly lower in the ED patients with CHF as compared to those with obstructive pulmonary disease.[3,4] In addition, using an algorithm including ETCO2 levels in addition to brain natriuretic peptide (BNP) has been shown to improve appropriate diagnosis by physicians in the pre-hospital setting. BNP and aminoterminal pro-BNP (NT-proBNP) have been proposed as early markers of HF and demonstrated to be useful for diagnosing and excluding HF in the ED. A combination of BNP or NT-proBNP testing and standard clinical assessment has been suggested to be superior to either tool used in isolation.
The purpose of this study is to investigate the relative clinical value and role of NT-proBNP and ETCO2 in the ED to differentiate HF from other causes of acute dyspnoea, especially COPD and sepsis with ARDS. We hypothesise that lower ETCO2 levels and higher NT-proBNP levels may predict HF versus obstructive pulmonary disease.
Objectives
The objectives of the study were as follows:
To measure NT-proBNP and ETCO2 in patients presenting with dyspnea
To evaluate the NT-proBNP and ETCO2 in patients of HF and COPD and other patients presenting with dyspnoea.
MATERIAL AND METHODS
Our study was a prospective, cross-sectional and observational study and was performed in Government Medical College and Hospital, Nagpur, between October 2019 and October 2021 in patients admitted to medicine intensive care unit and wards. The study was approved by the Institutional Ethical Committee. Informed written consent was taken from all the subjects or their relatives participating in the study.
The patients were further categorised into groups as per their clinical manifestations and investigation reports:
HF (n = 52)
Pulmonary (COPD – 29 and PE – 2)
Sepsis with ARDS (n = 13).
All patients underwent initial clinical examination with a recording of initial vital parameters along with on-admission ETCO2 measurement, NT-proBNP testing, arterial blood gas (ABG) testing, lung ultrasound examination, 2D echocardiography, chest X-rays, and other basic diagnostic laboratory testing.
RESULTS
A total of 96 patients presenting with dyspnoea requiring ventilatory support were included in the study. Of the 96 patients included in the study, 41 were male and 55 were female. The mean age of the patients was 54.73 ± 16.71 years with a minimum age of 21 years and a maximum age of 85 years
The HF group consisted of 52 patients (21 M/31 F) (54.2%) with a mean age of 52 ± 17.14 years, the pulmonary group included 31 patients (17 M/14 F) (32.3%) with a mean age of 61.06 ± 12.96 years and the sepsis with ARDS group included 13 patients (3 M/10 F) (13.5%) with a mean age of 50.54 ± 19.68 years
Systemic hypertension was found to be the most common comorbidity followed by diabetes mellitus, COPD, ischaemic heart disease, valvular heart disease, old pulmonary tuberculosis, and dyslipidaemia. No significant correlation was found between comorbidities and the study results
[Table 1] showing ABG, P/F ratio, ETCO2, and PaCO2-ETCO2 values in all study groups.
[Table 2] showing electrocardiographic, echocardiographic, and radiographic findings in all the groups [Figures 1 and 2].
Median NT-proBNP was found to be maximum for the HF group (11,480 pg/ml with an interquartile range of 12,564.75 pg/ml) followed by the sepsis group (780 pg/ml with an interquartile range of 2993.8 pg/ml) followed by the pulmonary group (231 pg/ml with an interquartile range of 216 pg/ml). The group-specific mean NT-proBNP in the HF group was 13,477.07 ± 9768.01 pg/ml followed by 4890.61 ± 9583.78 pg/ml in sepsis with the ARDS group and 467.10 ± 798.06 pg/ml in the pulmonary group. These results were statistically significant (P = 0.00). Median NT-proBNP values of all groups were less than mean values due to wide variation between maximum and minimum values of NT-proBNP values in a few patients in all the groups suggestive of outliers in the study groups. This difference in mean and median could be because of the presence of HF in these patients in addition to their primary diagnosis of sepsis/COPD/PE
The mean ETCO2 was observed to be maximum in the pulmonary group which was 48.61 ± 8.08 mmHg followed by the HF group with a mean ETCO2 of 31.52 ± 10.92 mmHg and the sepsis with the ARDS group with a mean ETCO2 of 19.46 ± 12.15 mmHg. This result was statistically significant (P = 0.00)
The mean PaCO2-ETCO2 was found maximum in the sepsis with the ARDS group as 16.79 ± 6.98 mmHg. The mean PaCO2-ETCO2 in the pulmonary group was 6.43 ± 2.72 mmHg and in the HF group was 5.52 ± 2.07 mmHg (least among all three groupsThis result was statistically significant (P = 0.00)
The study also included two patients with PE with a mean NT-proBNP of 13,649 ± 4240.52 pg/ml, mean ETCO2 of 29 ± 1.41 mmHg, and mean PaCO2-ETCO2 of 8.8 ± 2.55 mmHg [Table 1]
According to the above receiver operating characteristic (ROC) curve for NT-proBNP of all groups, the HF group [Figure 3] had the greatest area under the curve (AUC) of 0.944 compared to the pulmonary group [Figure 4] with an AUC of 0.037 and the sepsis group [Figure 5] with AUC of 0.407. Thus, the study showed AUC maximum for HF suggesting NT-proBNP as a better diagnostic marker for HF
| Parameters | Heart failure | Pulmonary | Sepsis with ARDS |
|---|---|---|---|
| ABG parameters | pH=7.37±0.12 pCO2=36.91±11.32 pO2=111.28±29.43 HCO3=21.35±6.73 |
pH=7.34±0.10 pCO2=54.98±8.11 pO2=77.35±22.68 HCO3=27.18±5.91 |
pH=7.30±0.12 pCO2=37.02±9.48 pO2=101.76±33.72 HCO3=17.8±6.98 AG=15.02±2.42 |
| SpO2 | 77±0.17% | 76±0.08% | 76±0.06% |
| PaO2/FiO2 | 198.18 | 105.73 | 183.52 |
| NT-proBNP | 11,480 pg/ml | 231 pg/ml | 780 pg/ml |
| ETCO2(mmHg) | 31.52±10.92 | 48.61±8.08 | 19.46±12.15 |
| PaCO2-ETCO2 | 5.52±2.07 mmHg | 6.43±2.72 mmHg | 16.79±6.98 mmHg |
| Heart failure | Pulmonary | Sepsis with ARDS | |
|---|---|---|---|
| ECG findings | ST-T changes/poor R wave progression/LVH/LBBB | COPD -RVH, RBBB P.E. -Sinus tachycardia, S1Q3T3 (n=2) |
Sinus tachycardia |
| Echo findings | RWMA and LV dysfunction (n=43); thrombosed prosthetic valve (n=3) | COPD -RA/RV dilated with mod. to sev. PAH and TR (n=9) Pulmonary embolism (P.E.) – D-shaped LV cavity, sev. TR, sev. PAH, free-floating RV thrombus, RA and RV dilated (n=2) [Figure 2] |
Mild LV hypokinesia, normal LVEF (n=6) |
| Lung USG findings | B lines pattern seen (comet tail sign) (n=44) [Figure 1] | A-lines present (n=31) | Shred sign (n=9) Sign of pleural effusion (n=4) |
| CXR findings | Bat wing opacities, Cardiomegaly | Signs of COPD | Diffuse B/L asymmetrical floccular or ground-glass opacities |

- Lung ultrasound image showing depicting showing comet tail sign (arrows).

- 2D Echocardiography right ventricle thrombus in pulmonary embolism.

- ROC curve for NT-proBNP, ETCO2 and PaCO2-ETCO2 in the heart failure group.

- ROC curve for NT-proBNP, ETCO2 and PaCO2-ETCO2 in the pulmonary group.

- ROC curve for NT-proBNP, ETCO2 and PaCO2-ETCO2 in the sepsis group.
While comparing the ROC curve for ETCO2 of all groups, the pulmonary group [Figure 4] had a maximum AUC of 0.914 as compared to the HF group [Figure 3] with an AUC of 0.318 and the sepsis group [Figure 5] with an AUC of 0.136 (least among all three groups). Thus, indicating ETCO2 as a better marker for diagnosing obstructive airway disease
According to the above ROC curves, the maximum AUC for PaCO2-ETCO2 was found in the sepsis group as 0.972 [Figure 5] as compared to AUC of 0.478 in the pulmonary group [Figure 4] and 0.291 in the HF group [Figure 3], thus indicating PaCO2-ETCO2 as a better marker for the detection of ARDS
In our study, the correlation between PaCO2 and ETCO2 as depicted in [Figure 6] was found to be 0.90, which indicated a strong positive correlation between PaCO2 and ETCO2 levels in all patients and was found to be statistically significant (P < 0.05). The linear correlation between HCO3 and ETCO2 as depicted in [Figure 7] was found as 0.620 which indicated a moderate positive correlation between HCO3 and ETCO2 and was found to be statistically significant (P < 0.05). The Bland and Altman plot in [Figure 8] showed the limit of the agreement between ETCO2 and PaCO2 as 7.92 mmHg and a precision of 6.20 mmHg with 95% C.I. (−4.24, 20.07). Ninety-two (95.83%) of the ETCO2 measurements were between 95% C.I. which indicates that the values of ETCO2 could be acceptable for clinical use
The lung ultrasound used for detecting B lines (comet tail sign) for diagnosis of HF showed sensitivity = 84.62%, specificity = 97.62%, positive predictive value (PPV) = 97.78% and negative predictive value (NPV) = 83.67% with accuracy = 90.43% and likelihood ratio of a positive test as 35.65 [Figure 1 and Table 2]. The NT-proBNP cutoff value was found to be 3942.5 pg/ml along with sensitivity = 90.38%, specificity = 92.86%, PPV = 94% and NPV = 88.63% for NTproBNP in diagnosis of HF patients. Thus, suggesting that lung ultrasound can be effectively used to exclude HF from pulmonary-related dyspnoeic patients along with positive NT-proBNP results and history of HF.
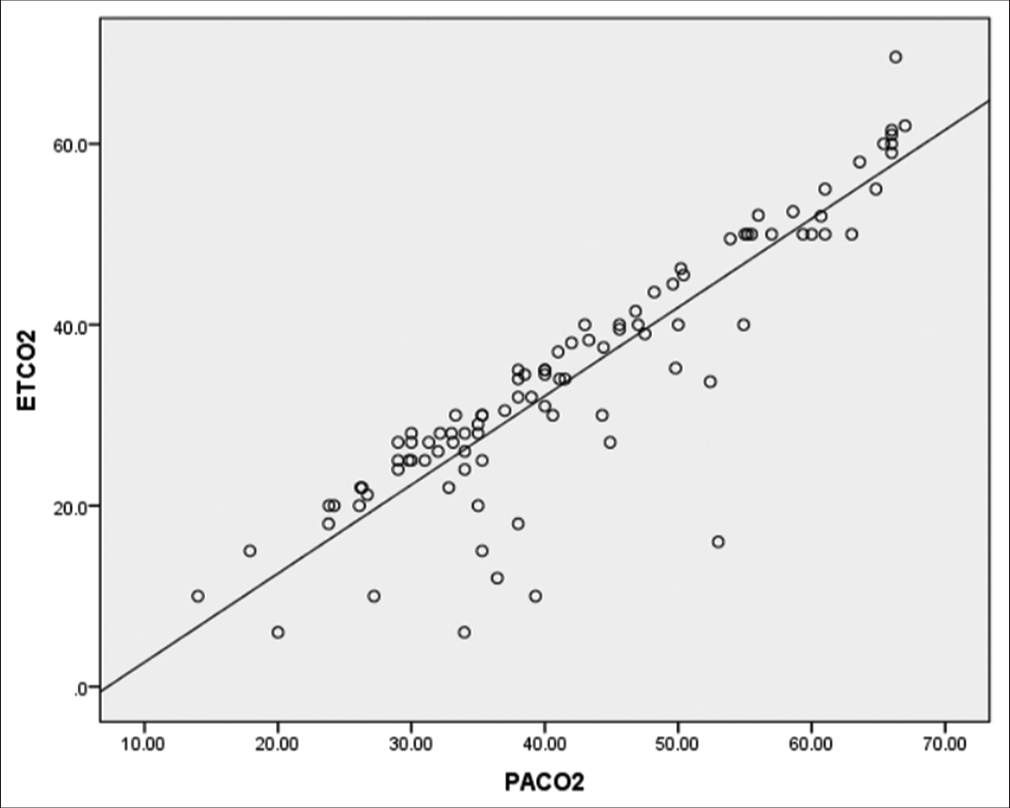
- Linear correlation between ETCO2 and PaCO2.

- Linear correlation between ETCO2 and HCO3.

- Bland-Altman plot of ETCO2 compared to PaCO2.
DISCUSSION
Our study (similarly to the study by Prosen et al.) suggests that NT-proBNP and ultrasound examinations provide diagnostic information useful in the early evaluation of HF in the emergency setting. Prosen et al.[5] study had mean NT-proBNP in the HF group as 2263±641.2 pg/ml and that in the pulmonary group was 598.2 ± 361.8 pg/ml with P = 0.008 with AUROC curve for NT-proBNP as 0.90 similar to the results found in our study. Prosen et al. study showed 100% sensitivity, 95% specificity, 96% PPV, 100% NPV, and a likelihood ratio of a positive test as 20 for the presence of B lines in lung ultrasound examination for the diagnosis of HF which are near to our study findings. Thus, the combination of ultrasound examination and rapid bedside NT-proBNP testing proves to be a reliable method for the identification of acute HF and its differentiation from COPD/asthma-related causes of acute dyspnoea. Klemen et al.[6] study had a mean NT-proBNP of 687.2 ± 479.5 pg/ml in the pulmonary-related dyspnoea group and 2756.8 ± 885.3 pg/ml in the acute HF-related dyspnoea group with P = 0.004 suggesting statistically significant importance of NT-proBNP in HF patients. The AUROC curve in this study for NT-proBNP was 0.90 (95% CI 0.85–0.94) which is close to the AUROC curve of our study in the HF group patients. Januzzi et al.[7] study results showed the median NT-proBNP concentration of patients with acute HF as 2844 pg/ml with an interquartile range of 1247–5976 pg/ml, which was substantially higher than those without acute HF who had a median NT-proBNP value of 98 pg/ml with an interquartile range of 35–369 pg/ml. The ROC curve for all patients demonstrated an AUC of 0.91 (95% CI: 0.90–0.93; P < 0.001) which is similar to our study’s AUROC value.
This study demonstrates that ETCO2 levels are lower in patients presenting with dyspnoea caused by HF, as compared with obstructive pulmonary disease. Prior studies such as Klemen et al.[6] and Hunter et al.[2] studies have similarly found that ETCO2 is lower in patients with CHF versus those with obstructive pulmonary disease and have also described using ETCO2 in conjunction with serum BNP to improve diagnostic accuracy in the pre-hospital setting.
Delerme et al.[8] study showed that the mean difference between PaCO2 and ETCO2 was 8 ± 10 mmHg, and the median value was 6 mmHg (with differences varying from −12 to 41 mmHg). The Bland and Altman plot showed limits of agreement (±1.96 of the difference) of −10 and +26 mmHg, with a mean of +8 mmHg. Using simple linear regression, the correlation between ETCO2 and PaCO2 was good (R = 0.82). This finding was found to be similar to that observed in our study.
Cinar et al.[9] study showed that ETCO2 measurement had a high correlation (r = 0.911) and agreement (0.5 ± 5 mmHg, between −10.5 and +9.5 mmHg) with PaCO2 levels. The mean ETCO2 level was 39.47 ± 10.84 mmHg and the mean PaCO2 level was 38.95 ± 12.27 mmHg. There was a positive, strong and statistically significant correlation between ETCO2 and PaCO2 which is similar to our study findings.
Thus, both NT-proBNP and ETCO2 used together help in the early diagnosis and treatment of HF and respiratory-related dyspnoea, leading to decreased morbidity and mortality in patients presenting with acute dyspnoea.
CONCLUSION
NT-proBNP has high diagnostic accuracy in differentiating acute HF-related dyspnoea from pulmonary-related acute dyspnea
Lower levels of ETCO2 were associated with CHF and higher levels of ETCO2 were observed in patients with respiratory causes of dyspnoea (COPD)
Higher PaCO2-ETCO2 value was found in patients with sepsis with ARDS and a high correlation was found between PaCO2 and ETCO2. Thus, capnography can be used for primary diagnosis of pulmonary disease patients and patients with metabolic acidosis in emergency wards however, the ABG must be considered the gold standard tool for diagnosis and guiding the treatment
Ultrasound examination of the lungs alone or in combination with NT-proBNP testing has high diagnostic accuracy in differentiating acute HF related from COPD/ asthma-related causes of acute dyspnoea in emergency settings
Therefore, both NT-proBNP and ETCO2 can help in patients presenting with acute dyspnoea for diagnosis and guiding further management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Acute respiratory failure in the elderly: Etiology, emergency diagnosis and prognosis. Critical Care. 2006;10:82.
- [CrossRef] [PubMed] [Google Scholar]
- Prehospital end-tidal carbon dioxide differentiates between cardiac and obstructive causes of dyspnoea. Emerg Med J. 2015;32:453-6.
- [CrossRef] [PubMed] [Google Scholar]
- End-tidal carbon dioxide monitoring in emergency medicine, Part 1: Basic principles. Acad Emerg Med. 1998;5:628-36.
- [CrossRef] [PubMed] [Google Scholar]
- Heart failure and chronic obstructive pulmonary disease: Diagnostic pitfalls and epidemiology. Eur J Heart Fail. 2009;11:130-9.
- [CrossRef] [PubMed] [Google Scholar]
- Combination of lung ultrasound (a comet-tail sign) and N-terminal probrain natriuretic peptide in differentiating acute heart failure from chronic obstructive pulmonary disease and asthma as cause of acute dyspnea in prehospital emergency setting. Crit Care. 2011;15:114.
- [CrossRef] [PubMed] [Google Scholar]
- Combination of quantitative capnometry, N-terminal pro-brain natriuretic peptide, and clinical assessment in differentiating acute heart failure from pulmonary disease as cause of acute dyspnea in pre-hospital emergency setting: Study of diagnostic accuracy. Croat Med J. 2009;50:133-42.
- [CrossRef] [PubMed] [Google Scholar]
- N-Terminal Pro-B-type natriuretic peptide in the emergency department the ICON-RELOADED study. J Am Coll Cardiol 208;. ;71:1191-200.
- [Google Scholar]
- Concordance between capnography and capnia in adults admitted for acute dyspnea in an ED. Am J Emerg Med. 2010;28:711-4.
- [CrossRef] [PubMed] [Google Scholar]
- Can mainstream end-tidal carbon dioxide measurement accurately predict the arterial carbon dioxide level of patients with acute dyspnea in ED. Am J Emerg Med. 2012;30:358-61.
- [CrossRef] [PubMed] [Google Scholar]






