Translate this page into:
Long-term Sequelae: Sheehan’s Syndrome Unveiled 12 Years Postpartum Haemorrhage Complicated by Pulmonary Tuberculosis – A Clinical Case Report
*Corresponding author: Gyanshankar Mishra, Department of Respiratory Medicine, Indira Gandhi Government Medical College, Nagpur, Maharashtra, India. gpmishra81@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shaikh MN, Mishra G, Munje RP, Gour S. Long-term Sequelae: Sheehan’s Syndrome Unveiled 12 Years Postpartum Haemorrhage Complicated by Pulmonary Tuberculosis – A Clinical Case Report. Vidarbha J Intern Med. 2023;33:107-10. doi: 10.25259/VJIM_6_2024
Abstract
Sheehan’s syndrome, a rare but significant endocrinopathy, often emerges in the backdrop of severe postpartum haemorrhage and can remain undiagnosed for years. Primary care physicians play a crucial role in suspecting and diagnosing this condition, especially in women presenting with a history of puerperal haemorrhage, lactation failure and amenorrhea. The syndrome’s potential to cause life-threatening adrenal crises during episodes of acute illness, such as infections or pulmonary tuberculosis, underscores the need for vigilance and prompt intervention in affected individuals. This report highlights the case of a 35-year-old female who was diagnosed with Sheehan’s syndrome a notable 12 years after experiencing a severe postpartum haemorrhage. Her condition was eventually unmasked following her affliction with pulmonary tuberculosis, emphasising the complexity and delayed presentation of this syndrome. This case underscores the critical need for heightened awareness among healthcare professionals for early identification and management of Sheehan’s syndrome to prevent serious complications.
Keywords
Sheehan’s syndrome
Postpartum haemorrhage
Pulmonary tuberculosis
Addisonian crisis
Hypopituitarism
Pituitary necrosis
INTRODUCTION
Sheehan’s syndrome, a rare but significant complication of severe postpartum haemorrhage, manifests as hypopituitarism due to ischemic necrosis of the pituitary gland. This syndrome’s clinical presentation can vary greatly, with some individuals remaining asymptomatic for prolonged durations without the need for hormone replacement therapy. This variability underscores the importance of physicians maintaining a high degree of vigilance for potential acute stress-induced adrenal crises in undiagnosed cases of Sheehan’s syndrome. The early detection of this syndrome is essential, necessitating increased clinical awareness, particularly in patients with a history of severe postpartum haemorrhage.[1]
Sheehan’s syndrome results from ischemic necrosis affecting the anterior pituitary gland, which occurs subsequent to significant postpartum haemorrhage. The clinical manifestations of Sheehan’s syndrome are diverse and are related to hypopituitarism and secondary adrenal insufficiency. The insidious progression of endocrinological abnormalities often leads to delayed diagnosis, attributable to the non-specific nature of associated symptoms, including fatigue, weight loss, nausea, fever, abdominal pain and myalgia.[2-5]
While recent advancements in obstetric care have reduced the incidence of Sheehan’s syndrome, its exact prevalence remains uncertain, largely due to a considerable number of undiagnosed cases. This uncertainty highlights the imperative for enhanced diagnostic vigilance and postpartum care.[6]
According to data from the World Health Organization, it is estimated that annually around 100,000 women globally succumb to complications related to Sheehan’s syndrome. Moreover, in 1996, over 3 million women worldwide were affected by this condition. Notably, the syndrome is frequently overlooked, even in developed countries, leading to diagnostic delays that can extend up to 48 years.[2-5,7,8]
An adrenal crisis, which can arise from conditions such as Sheehan’s syndrome, represents a life-threatening medical emergency that requires immediate intervention.[9] This case report discusses a patient who, 12 years following a severe postpartum haemorrhage, presented with an adrenal crisis induced by an infection with Mycobacterium tuberculosis.
This patient’s Sheehan’s syndrome had remained undiagnosed and untreated until this critical event, highlighting the challenges and implications of delayed diagnosis in this complex clinical scenario.
CASE REPORT
We present a case involving a 35-year-old married female who was admitted to exhibiting symptoms including fever, cough, generalised weakness, dyspnoea, vomiting, headache and altered mental status for one week. The patient had been receiving antitubercular therapy for reactivated pulmonary tuberculosis diagnosed at another hospital for the past month. Her medical history was notable for an episode of pulmonary tuberculosis at the age of 16 years, though specific details were unavailable. A significant finding was her 12-year history of amenorrhea. Further, detailed history-taking revealed that her husband reported a severe postpartum haemorrhage secondary to puerperal sepsis caused by retained gauze during childbirth, followed by massive blood transfusion and surgical intervention. Post-delivery, she experienced lactation failure, continued amenorrhea and secondary infertility. In addition, she had recurrent episodes of dyspepsia and gastroenteritis, which resolved with unspecified medications. There was no history of head trauma, surgical interventions, radiation exposure, polyuria or polydipsia.
On physical examination, the patient was conscious but displayed confusion and a lack of cooperation. Her body mass index was 16.01 kg/m2, with a pulse rate of 108 beats/ min, blood pressure measured at 80/50 mmHg and oxygen saturation at 98% on room air. She exhibited slight conjunctival pallor, no scleral icterus, absent neck rigidity and unremarkable bilateral fundoscopy. Bilateral lung crepitations were noted on auscultation, and the cardiac examination was normal except for tachycardia.
Laboratory investigations revealed persistent hyponatremia, as shown in Table 1, with serum sodium and potassium levels fluctuating over the period from 27 February to 16 March. Arterial blood gas analysis indicated a pH of 7.411, partial pressure of carbon dioxide of 34.40 mmHg, partial pressure of oxygen of 115.5 mmHg, bicarbonate levels at 22.81 mmol/L, a base excess of −2.01 mmol/L and an anion gap of 17.6 mmol/L. Additional tests showed a random blood sugar level of 73 mg/dl, negative results for M. tuberculosis in sputum and gastric aspirate, negative blood culture, negative dengue immunoglobulin M, elevated D-dimer levels at 516.8 ng/mL, increased serum lactate dehydrogenase at 727 U/L, elevated serum C-reactive protein at 38 mg/dL, urine protein at 107 mg/dL and urine creatinine at 24 mg/dL. Thyroid function tests revealed significantly reduced levels of Free T3 and Free T4 with a thyroid-stimulating hormone level of 3.17 mIU/mL. Serum prolactin was measured at 1.55 ng/mL, below the normal range.
| Serum sodium-Na (mEq/L) |
Serum potassium-K (mEq/L) | ||
|---|---|---|---|
| 27/02/2023 | 120 | 3.8 | |
| 30/02/2023 | 113.4 | 3.73 | |
| 03/03/2023 | 123.5 | 2.92 | |
| 06/03/2023 | 112.6 | 4.5 | |
| 09/03/2023 | 108 | 4.5 | |
| 10/03/2023 | 118.9 | 4.32 | |
| 13/03/2023 | 99.1 | 4.3 | |
| 14/03/2023 | 119.2 | 4.5 | |
| 16/03/2023 | 120.5 | 4.23 | |
Chest radiograph PA view [Figure 1] revealed right upper zone and mid-zone fibrosis suggestive of post-tuberculosis sequelae.

- Chest radiograph PA view (14 March 2023).
Non-contrast computed tomography of the head indicated pansinusitis without other abnormalities. Ultrasonography of the thorax and abdomen revealed bilateral minimal pleural effusion and mild inter-bowel collection, with an atrophied uterus and non-visualisable bilateral ovaries.
Plain magnetic resonance imaging (MRI) of the brain [Figure 2], conducted using a 3T MRI machine with various sequences, showed a widened sella turcica filled with cerebrospinal fluid, a thin residual rim of pituitary parenchyma measuring <1 mm in height and an absent posterior pituitary bright spot. These features are indicative of secondary empty sella. The pituitary stalk appeared normal. These MRI findings, combined with her history of postpartum haemorrhage, strongly suggested sequelae to pituitary apoplexy, consistent with Sheehan’s syndrome.
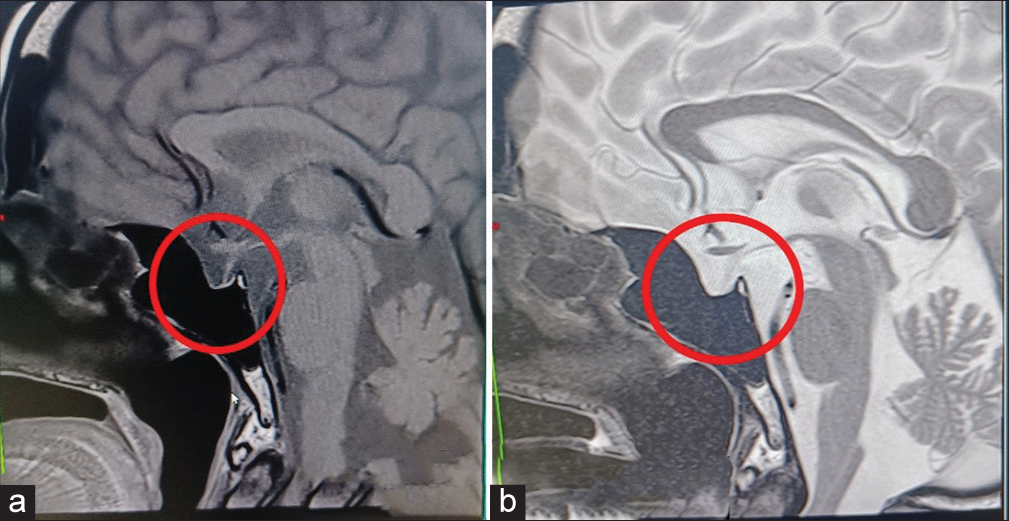
- Magnetic resonance imaging (MRI) scan of the brain (a) showing T1 and (b) T2 images (11 March 2023) showing empty sella (red circles).
The patient received treatment with injectable hydrocortisone in divided doses, which was then tapered to oral steroids. Before discharge, hormonal therapy was initiated, including dexamethasone (4 mg daily) and thyroxine (50 mg daily).
DISCUSSION
The present case report highlights a patient with Sheehan’s syndrome, an unexpected diagnosis that was unmasked following an adrenal crisis triggered by pulmonary tuberculosis. This case brings to light several key clinical aspects. First and foremost, it demonstrates that some individuals with Sheehan’s syndrome may endure extended periods without the necessity for hormone replacement therapy. This observation points to the diverse severity and progression of hypopituitarism associated with the syndrome.[9] In addition, it is noted that infections such as pulmonary tuberculosis, or the use of rifampicin in anti-tuberculosis treatment, can serve as catalysts for adrenal crises in cases of subclinical adrenal insufficiency, as exemplified by our patient’s experience with Sheehan’s syndrome.[10]
A critical lesson from this case is the importance of a comprehensive medical history, particularly focusing on postpartum events, to identify women potentially at risk for Sheehan’s syndrome. Remarkably, our patient had lived for over 12 years without hormonal replacement, without encountering any significant health issues, reflecting the often subtle and variable clinical presentation of Sheehan’s syndrome. This delayed diagnosis can be ascribed to the gradual progression of hormone deficiencies, where partial hypopituitarism might permit some patients to function without immediate hormone replacement therapy.
This case report suggests that an effective approach for early detection involves a meticulous review of the patient’s medical history, emphasising factors such as lactation failure and the resumption of menstrual cycles postpartum. Furthermore, it highlights the critical need for prompt initiation of glucocorticoid therapy in suspected cases of Sheehan’s syndrome, even before the confirmation of diagnosis through testing. The therapeutic management of Sheehan syndrome, similar to general hypopituitarism, is primarily focused on hormone replacement therapy. Crucially, in treating Sheehan syndrome, it is vital to begin glucocorticoid replacement before administering thyroid hormones to reduce the risk of precipitating an adrenal crisis, thereby ensuring the safe correction of endocrine imbalances and lowering mortality risks associated with this condition.
This case also sheds light on the possible partial functionality of the patient’s atrophic adrenal glands before her hospitalisation and speculates how the infection with pulmonary tuberculosis or the rifampicin-based therapy may have induced the adrenal crisis. In conclusion, this case underscores the imperative for increased awareness among healthcare providers to enable early detection and effective management of Sheehan’s syndrome.[1]
CONCLUSION
In the intricate landscape of women’s health, the recognition and prompt diagnosis of infrequent yet significant conditions like Sheehan’s syndrome are of paramount importance, necessitating a heightened level of vigilance among primary care physicians. This sense of urgency is particularly pertinent given its correlation with a medical history characterised by puerperal haemorrhage, lactation failure and sustained amenorrhea. Furthermore, the subtle and often deceptive clinical manifestations of Sheehan’s syndrome, which can escalate into an adrenal crisis, demand careful consideration. This is especially true in scenarios where patients exhibit sudden changes in mental status, hypotension, fever and hypoglycaemia during episodes of acute illness, such as viral infections or conditions like pulmonary tuberculosis, potentially years after the initial postpartum event.
The process of diagnosing Sheehan’s syndrome relies heavily on a thorough and insightful evaluation of the patient’s medical history, complemented by a detailed physical examination and strategic use of pertinent laboratory tests. This comprehensive and multi-dimensional approach is crucial for demystifying the complexities inherent in Sheehan’s syndrome. It underscores the essential role of healthcare practitioners in maintaining an ongoing state of alertness and preparedness to recognise and address rare, yet impactful, medical conditions within their clinical practice. Such vigilance not only enhances patient outcomes but also contributes significantly to the broader understanding and management of these challenging medical phenomena.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The Adrenal Crisis Precipitated by Influenza A Led to the Diagnosis of Sheehan's Syndrome 18 Years after Postpartum Hemorrhage. Clin Case Rep. 2020;8:3081-6.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristic Features of 20 Patients with Sheehan's Syndrome. Gynecol Endocrinol. 2006;22:279-83.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent Hypoglycaemia: A Delayed Presentation of Sheehan Syndrome. Case Rep. 2014;2014:bcr2013200991.
- [CrossRef] [PubMed] [Google Scholar]
- Four Decades without Diagnosis: Sheehan's Syndrome, a Retrospective Analysis. Gynecol Endocrinol. 2016;32:904-7.
- [CrossRef] [PubMed] [Google Scholar]
- Extensive Investigation of 114 Patients with Sheehan's Syndrome: A Continuing Disorder. Eur J Endocrinol. 2014;171:311-8.
- [CrossRef] [PubMed] [Google Scholar]
- A Case of Sheehan's Syndrome Associated with Severe Anemia and Empty Sella Proved 48 Years after Postpartum Hemorrhage. Endocr J. 1995;42:803-9.
- [CrossRef] [PubMed] [Google Scholar]
- Sheehan's Syndrome of more than 30 Years' Duration: An Endocrine and MRI Study of 6 Cases. Endocr J. 1998;45:451-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adrenal Crisis: Still a Deadly Event in the 21st Century. Am J Med. 2016;129:339.e1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Rifampicin-induced Adrenal Crisis in a Patient with Tuberculosis: A Therapeutic Challenge. BMJ Case Rep. 2016;2016:bcr2016216302.
- [CrossRef] [PubMed] [Google Scholar]






