Translate this page into:
Study of Clinical Spectrum of Neurological Manifestations in HIV/AIDS Seen at Tertiary Referral Hospital in India
*Corresponding author: Dr. Kiran Bhagwat, Department of Neurology, Command Hospital (EC), Kolkata, India. kiranbhagwat2000@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhagwat K, Yegade W, Singh J, Meshram A, Goel J. Study of Clinical Spectrum of Neurological Manifestations in HIV/AIDS Seen at Tertiary Referral Hospital in India. Vidarbha J Intern Med. 2023;33:82-9. doi: 10.25259/VJIM_5_2024
Abstract
Objectives:
The pandemic caused by human immunodeficiency virus (HIV) is one of the fastest growing health problems in the world today. Neurological manifestations of HIV infection and acquired immunodeficiency syndrome (AIDS) are being seen in a frequency that is parallel to the increasing number of new cases seen the world over. The World Health Organisation (WHO) estimates that 36.7 million people in the world are infected with HIV. Neurological manifestations of HIV disease can be seen in 20% of outpatients in HIV clinics and almost half of HIV patients being treated as in-patients. Of the various subtypes of HIV, subtype C is responsible for more than 50% of HIV1 infections causing rapidly growing epidemics in India. The objectives of this study were as follows: (1) To evaluate the prevalence of neurological manifestation in HIV-positive patients admitted to a tertiary referral Hospital in India. (2) To describe the neurological manifestations documented. (3) To find the possible predictors of neurological manifestations.
Material and Methods:
This study was a single centre prospective cross-sectional study in which out of 200 HIV/AIDS patients, 40 patients with neurological manifestations were analysed over a period of 18 months. They were interviewed and evaluated with particular reference to neurological manifestations, and were classified using the WHO staging system.
Results:
Amongst the studied population of 40 patients, 16 patients (40%) manifested as tuberculous meningitis (TBM) with or without brain tuberculomas, followed by seven patients (18%) presented with peripheral neuropathy and six patients (15%) presented with central nervous system (CNS) vasculitic or multi-infarct state. Cryptococcal meningitis was seen in five patients (12%), efavirenz-induced psychosis/seizure seen in one patient, while HIV-induced polymyositis, progressive multifocal leukoencephalopathy progressive multifocal leukoencephalopathy, acute inflammatory demylinating polyradiculoneuropathy, AIDS dementia complex and CNS toxoplasmosis were seen in one patient each respectively. One patient presented with dual opportunistic infection with coexistence of cryptococcal and tuberculous meningitis.
Conclusion:
Headache with or without vomiting, seizures and altered sensorium were the most common neurological symptoms. Fundus abnormalities, meningeal signs, gait abnormalities, cranial nerve dysfunction and hemiplegia were the most common neurological signs. New-onset headache was a significant predictor of the occurrence of neurological complications. Opportunistic infections such as TBM and Cryptococcal meningitis were most commonly observed.
Keywords
Progressive multifocal leukoencephalopathy (PMLE)
AIDS dementia complex (ADC)
Tuberculous meningitis (TBM)
Acute inflammatory demyelinating polyradiculoneuropathy (AIDP)
Acquired immunodeficiency syndrome (AIDS)
INTRODUCTION
Human immunodeficiency virus (HIV)-1 is a neurotropic virus.[1] In a resource-limited country such as India, large populations of affected patients now have access to adequate chemoprophylaxis for opportunistic infections (OIs), allowing them to live longer. With the identification of HIV in 1983 and its proof as etiologic agent in 1984 and with the availability of sensitive and specific diagnostic tests for HIV infection, the case definition of acquired immunodeficiency syndrome (AIDS) has undergone several revisions over the years. The current Centre of Disease Control (CDC) classification system for HIV-infected adolescents and adults categorises persons based on the clinical conditions associated with HIV and CD4 counts. Using this system, any HIV-infected individual with a CD4 count of <350/mm3 has AIDS by definition regardless of the presence of symptoms or opportunistic diseases. The pandemic caused by HIV is one of the greatest public health threats in the world today.[2] It is estimated that one million are thought to have died of the illness by December 2016, while another 36.7 million HIV-infected people were alive. Almost 1.8 million people are thought to have been infected during the previous 12 months. The majority of the disease burden remains in sub-Saharan Africa, but the number of HIV-infected people is rapidly increasing in other regions, especially in Asia and Eastern Europe.
HIV is predominantly transmitted sexually, but other routes of transmission include parenteral transmission–through infected blood, blood products or injecting drug use and vertical transmission from mother to child transmission, which may occur before, during or after birth. Although the complementary nature of preventing new HIV infections and treatment and care of HIV-infected individuals was recognised some time ago, only recently has it been more widely recognised that the containment of the HIV pandemic requires a global strategy which combines effective prevention with treatment and care programmes. The increased provision of HIV treatment, care and prevention services to millions of HIV-infected people have now become a HIV major policy target among national and international organisations across the world.
The hallmark HIV disease is profound immunodeficiency resulting primarily from progressive qualitative and quantitative deficiency of a subset of T lymphocytes referred to as helper T-cells or inducer T-cells. This subset of T-cells is defined phenotypically by the presence on its surface of CD4 molecule which serves as a primary cellular receptor for HIV. When the number of CD4 cells decline below a certain level, the patient is at high risk for developing a variety of opportunistic diseases particularly the infections and neoplasia that are AIDS-defining illnesses.[3] The diagnosis of HIV infection depends on the demonstration of antibodies to HIV and/or the direct determination of HIV or one of its components. The standard screening test for HIV infection is enzyme-linked immunosorbent assay (ELISA) and the most common confirmatory test is the Western blot. The CD4+ T-cell is the laboratory test considered as the best indicator of immunologic competence of patients with HIV infection.
It is now recognised that every level of the neuroaxis can be involved and at least 1/3 of the patients with advanced HIV infections will develop neurological complications during the course of their illness and in 10% of the cases, it may be first sign of the development of AIDS.[4]
Neurological manifestations related to HIV infection can be broadly classified into HIV infection, OI, neoplasia and antiretroviral therapy (ART) related.[5]
HIV estimates derived using globally comparable methods and findings from the independent Impact Assessment Study show that the National AIDS Control Programme is progressing steadily toward the objective of halting and reversing the HIV epidemic in India over the period 2012-2017.[6] Available evidence on HIV prevalence and future statistical projections shows signs of stabilisation of HIV epidemic in India at national level. Provisional estimates show that there are 21.17 lakh people living with HIV/AIDS in India by the end of 2015 with an estimated adult HIV prevalence of 0.26%.
Declining trends are noted in high prevalence states indicating possible impact of sustained programme interventions. Even the prevalence among pregnant women in the age group of 15-24 years, which is considered proxy for incidence/new infections in general population, is showing a declining trend. The overall HIV prevalence among different population groups in 2014-15 continues to portray the concentrated epidemic in India, with a very high prevalence among high-risk groups-intravenous drug users (IDU’s) (9.9%), male sex with male (MSM) (7.3%), female sex workers (FSW’s) (4.3%) and sexually transmitted diseases (STD’s) clinic attendees (2.5%) and low prevalence among antenatal (ANC) clinic attendees (0.49%).
MATERIAL AND METHODS
Setting
This was a single centre non-randomised observational study between January 2012 and June 2013 on 40 out of 200 total HIV/AIDS patients in different stages of neurological manifestations seen as inpatients in a tertiary referral hospital in India. All respondents were adults, aged more than 18years. Informed consent was taken before inclusion in the study. Those who did not give consent for the study were excluded from the study.
Aims
This study is designed to evaluate various spectrums of neurological manifestations seen in HIV/AIDS patients seen at a tertiary referral hospital in India.
Objectives
The objectives of this study were as follows:
Primary
To evaluate the prevalence of neurological manifestation in HIV-positive patients admitted to a tertiary referral hospital.
To describe the neurological manifestations documented.
Secondary
To find the possible predictors of neurological manifestations.
To evaluate the neurological complications secondary to ART.
Methods
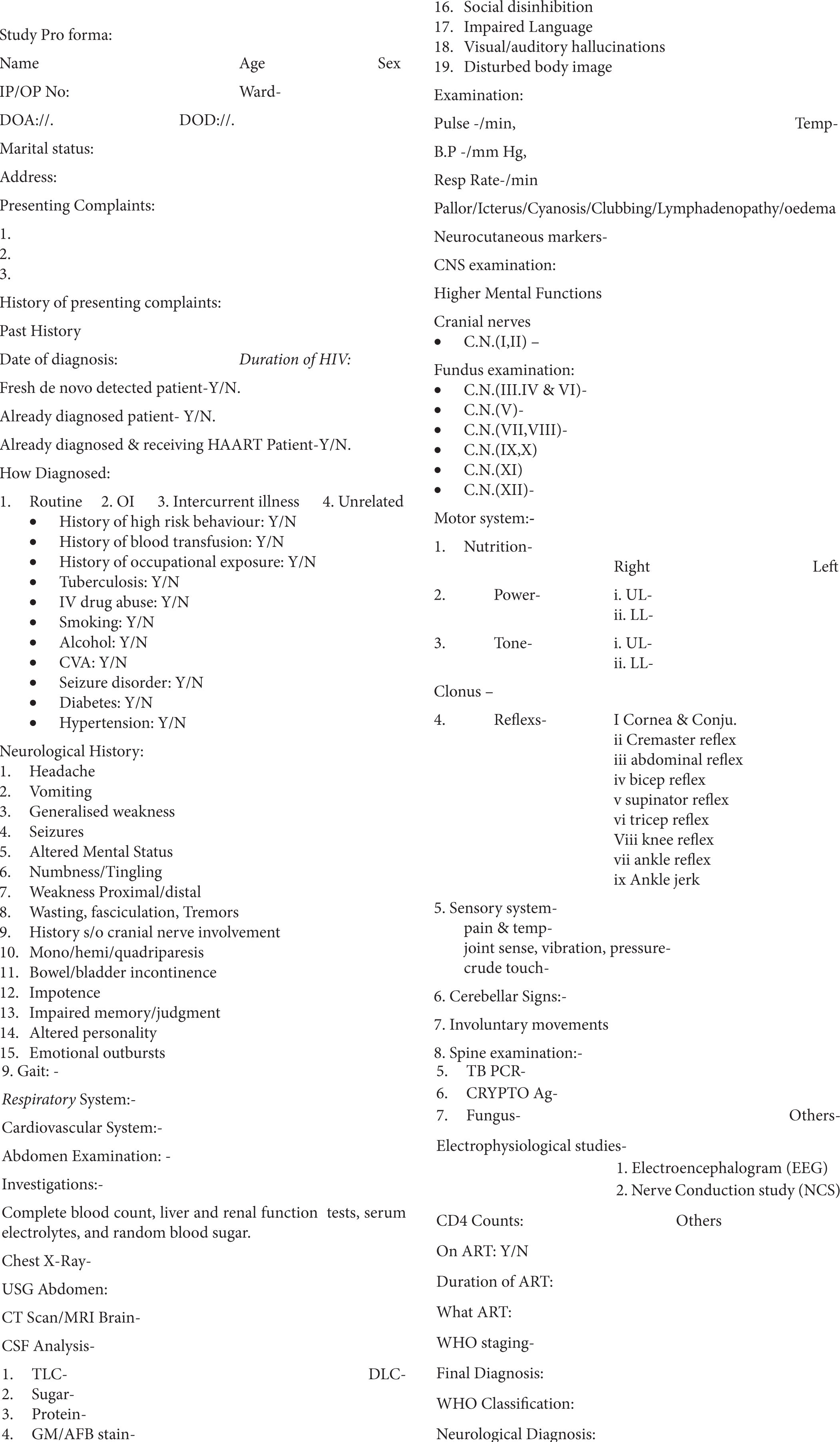
The study was a prospective cross-sectional study in which out of 200 HIV patients 40 patients with neurological manifestations were analysed. Patients were selected on an in-patient basis. All patients/attendants (in case of altered mental status) were interviewed face to face and evaluated by the investigator, with particular reference to neurological manifestations. Investigations were done based on the needs of the patients after a thorough clinical evaluation. They were classified into various stages of HIV using the World Health Organisation (WHO) staging system.
A Pro forma, which is appended in the Annexure, was used for the above purpose.
Tests
HIV was confirmed by the ELISA test. Total count and differential count were performed in the laboratory using automated counting chambers and confirmed manually. CD4 counts were analysed using the flow cytometry method -FACS calibur. Other tests including plasma viral load were done as per the needs of the patients.
Inclusion criteria
The following criteria were included in the study:
Patient those who are HIV-positive with neurological symptoms or signs at the time of admission or developed during hospital stay.
Exclusion criteria
The following criteria were excluded from the study:
HIV patients without neurological manifestations, pregnant lady patients or those who had not given consent for inclusion in study group.
Neurological manifestations due to other established causes such as ischemic/haemorrhagic stroke.
RESULTS
Mean age in males was 37years and in females 35years. The females had a shorter duration of HIV illness as compared to their male counterparts. Majority of the patients were diagnosed in a symptomatic state when they presented with an OI.[7] A greater proportion of females were diagnosed with HIV in an asymptomatic state during screening, either during pregnancy or when the spouse was found to be positive.
Almost 20% of patients were diagnosed recently with their first neurological manifestations. Half of the total patients presented within one year of illness. One patient presented as long as 15 years of their illness with neurological manifestations. A major risk factor for disease acquisition was unprotected sexual intercourse in 67% of our patients. About 21% of patients gave a history of blood transfusion, while 2% of the patients gave a history of occupational exposure (needle stick injury).
Approximately 70% of our patients gave a history of smoking, followed by 65% of patients who gave a history of significant alcohol consumption (>10 drinks per week). All the patients were male.
Headache was the most common neurologic symptom seen and was often associated with vomiting. This was followed by seizures and altered sensorium [Table 1].
| Symptoms | Frequency(n) | (%) |
|---|---|---|
| Headache | 17 | 42% |
| Vomiting | 11 | 28% |
| Altered Sensorium | 13 | 33% |
| Seizures | 5 | 13% |
| Impaired Judgement | 2 | 5% |
| Forgetfulness | 2 | 5% |
| Emotional outbursts | 3 | 7% |
| Impaired language | 2 | 5% |
| Hallucinations | 1 | 3% |
| Dreaming | 1 | 2% |
| Involvement of Cranial Nerve/s | 9 | 23% |
| Unilateral upper and lower limb | 4 | 10% |
| weakness | ||
| Bilateral lower limb weakness | 3 | 7% |
| Muscle pain | 2 | 5% |
| Wasting, Fasciculations | 0 | - |
| Limb weakness | 1 | 2% |
| Tingling and Numbness | 7 | 18% |
| Tremors | 1 | 2% |
| Ataxia | 2 | 5% |
| Bowel / Bladder symptoms | 2 | 5% |
| Impotence | 3 | 7% |
Fundus abnormalities were the most common neurological signs documented in 23patients. Other signs include meningeal signs, gait abnormalities, cranial nerve abnormalities and hemiplegia [Table 2].
| Signs | (%) |
|---|---|
| Fundus abnormality | 35 |
| Meningeal signs | 30 |
| Cranial nerve involvement | 23 |
| Paresthesia | 18 |
| Gait abnormality | 15 |
| Hemiparesis | 13 |
| Loss of consciousness | 10 |
| MMSE score less than (24/30) | 9 |
| Paraparesis | 5 |
| Cerebellar signs | 5 |
| Quadriplegia | 3 |
| Anisocoria | 3 |
MMSE: Mini mental status examination
The mean CD4 counts in males were 121.7/mm3 and in females 119.7/mm3.
Investigations
1. Cerebrospinal fluid (CSF) analysis [Figure 1]
![Cerebrospinal fluid (CSF) analysis. [TBM: tuberculous meningitis].](/content/140/2023/33/2/img/VJIM-33-082-g001.png)
- Cerebrospinal fluid (CSF) analysis. [TBM: tuberculous meningitis].
CSF analysis[8-10] was diagnostic in 22(84.61%) patients out of 26patients who underwent CSF analysis and tuberculosis followed cryptococcus was most frequent opportunistic infection noted amongst the studied population.
2. Computed tomography (CT)/Magnetic resonance imaging (MRI) brain findings [Figure 2]
![Computed tomography/magnetic resonance imaging brain findings among the studied patients. [SOLs: space occupying lesions].](/content/140/2023/33/2/img/VJIM-33-082-g002.png)
- Computed tomography/magnetic resonance imaging brain findings among the studied patients. [SOLs: space occupying lesions].
Cerebral edema was the most common brain imaging finding noted in 23% of patients, followed by space occupying lesions (SOLs)/basal exudates seen in 15% of patients, multiple infarcts were seen in 13% of patients, cerebral atrophy was noticed in 7% of patients, periventricular hyperintensity seen in 5% and hydrocephalus was seen in 5% of our patients. In 19% of patients, imaging was normal. Most of the space-occupying lesions detected were tuberculomas in disseminated tuberculosis patients, while one patient had toxoplasmosis.
Neurological diagnosis
Varied spectrum of neurological manifestations [Figure 3] was noted in 82% of the studied population and all the patients those had central nervous system (CNS) manifestations were in WHO stage 4. Fifty-five percent of the patients were on ART and the mean duration of ART was 19.84 months. Some of the patients were on the second or third line of ART. More than 25% of patients were detected recently. The CD4 counts showed better correlation with the occurrence of neurological manifestations.
![Spectrum of various neurological manifestations amongst human immunodeficiency virus/acquired immunodeficiency syndrome patients. [TBM: tuberculous meningitis, CVA: cerebrovascular accident, CNS: central nervous system, AIDP: acute inflammatory demyelinating polyradiculoneuropathy, ADC: AIDS dementia complex, PMLE: progressive multifocal leukoencephalopathy]. The numbers in bracket on the X-axis represent number of cases.](/content/140/2023/33/2/img/VJIM-33-082-g003.png)
- Spectrum of various neurological manifestations amongst human immunodeficiency virus/acquired immunodeficiency syndrome patients. [TBM: tuberculous meningitis, CVA: cerebrovascular accident, CNS: central nervous system, AIDP: acute inflammatory demyelinating polyradiculoneuropathy, ADC: AIDS dementia complex, PMLE: progressive multifocal leukoencephalopathy]. The numbers in bracket on the X-axis represent number of cases.
Type of ART
Among all the patients were not (45%) on ART, while those patients who were on (55%) ART were as follows [Figure 4]:
![Type of antiretroviral therapy. [TDF: tenofovir disoproxil fumarate, 3TC: lamivudine, EFZ: efavirenz, d4T: stavudine, NVF: nevirapine, TNF: tenofovir, FTC: emtricitabine, DAR+R: darunavir+ ritonavir].](/content/140/2023/33/2/img/VJIM-33-082-g004.png)
- Type of antiretroviral therapy. [TDF: tenofovir disoproxil fumarate, 3TC: lamivudine, EFZ: efavirenz, d4T: stavudine, NVF: nevirapine, TNF: tenofovir, FTC: emtricitabine, DAR+R: darunavir+ ritonavir].
on 1st line ART-15%,
2nd line ART-22%
3rd line ART-18%
Graphical correlation between CD4 count and neurological manifestations
Association between CD 4 count and neurological complications [Figure 5].
![Associations between CD4 count and neurological complications. [P. neuropathy: peripheral neuropathy, TBM + crypto M.: tuberculous meningitis + cryptococcal meningitis, EFZ: efavirenz, CNS: central nervous system, PMLE: progressive multifocal leukoencephalopathy, ADC: AIDS dementia complex, AIDP: acute inflammatory demyelinating polyradiculoneuropathy].](/content/140/2023/33/2/img/VJIM-33-082-g005.png)
- Associations between CD4 count and neurological complications. [P. neuropathy: peripheral neuropathy, TBM + crypto M.: tuberculous meningitis + cryptococcal meningitis, EFZ: efavirenz, CNS: central nervous system, PMLE: progressive multifocal leukoencephalopathy, ADC: AIDS dementia complex, AIDP: acute inflammatory demyelinating polyradiculoneuropathy].
DISCUSSION
Out of the total 200 HIV patients (outpatients + in-patients department) who came to our centre, neurological problem was detected in 40 patients. Headache with or without vomiting, seizures and altered sensorium were the most common neurological symptoms.[11-13] Fundus abnormalities, meningeal signs, gait abnormalities, cranial nerve dysfunction and hemiplegia were the most common neurological signs. New-onset headache was a significant predictor of the occurrence of neurological complications. CSF examination revealed a positive diagnosis in the majority of the patients who underwent the test. OIs remained the most common problems detected, which included tuberculous meningitis (TBM), Cryptococcal meningitis, a combination of both and viral meningitis.
HIV-related neurological problems documented (6 out of 40) included AIDS dementia complex,[14,15-17] neuropathy, progressive multifocal leukoencephalopathy, central nervous system vasculitis and seizures due to efavirenz.[18] One patient had coexistent TBM and cryptococcal meningitis, emphasising the need for clinicians to be aware that multiple OIs can exist in the same system in these patients.
Patients in WHO stage 4 were at the maximum risk for neurological complications. CD4 counts were significantly lower in patients with neurological complications, and most of the neurological manifestations and all the OIs were documented in the patients with CD4 counts below 350/mm3. Neurological complications did not show any correlation with the patients being on ART or with the duration of ART.[19,20] The possible reasons for this include differing baseline CD4 counts at the start of ART and treatment failure in a subset of patients.
CONCLUSION
Headache with or without projectile vomiting, altered sensorium, and seizure were the commonest symptoms, whereas fundus abnormalities, including papilledema, cranial nerve deficit, signs of meningeal irritation, and focal neuro-deficit in the form of hemiplegia were the commonest signs of neuro-axial involvement. New onset headache was a significant predictor of the occurrence of neurological complications. Amongst all the opportunistic infections (OI’s), tuberculosis, followed by cryptococcal, was the leading infectious etiology. Hence, we should have a low threshold in identifying and prompt treatment of such opportunistic infections for a better outcome in such a subset of patients.
Acknowledgments
The author sincerely thanks to all his colleagues, respected teachers, family members for their constant support, motivation and guidance.
Ethical approval
The research/study had been approved by the Institutional Review Board at Medicity Hospitals, Hyderabad (Telangana), vide reference number 111-12128-111-100110, dated 08 September 2011.
Declaration of patient consent
The auther certifies that he has obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Human Immunodeficiency Virus disease: AIDS and Related Disorders In: Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J, eds. Harrison’s Principles of Internal Medicine (19th ed). NewYork: McGraw-Hill; 2015.
- [Google Scholar]
- AIDS Epidemic Update: May 2016 UNAIDS/04.45E Geneva, Switzerland: UNAIDS/WHO; 2016.
- [Google Scholar]
- Neurological Complications of Acquired Immune Deficiency Syndrome: Analysis of 50 Patients. Ann Neural. 1983;14:403-18.
- [CrossRef] [PubMed] [Google Scholar]
- Neurological Manifestations of the Acquired Immune Deficiency Syndrome: Experience at UCSF and Review of the Literature. J Neurosurgeon. 1985;62:475-95.
- [CrossRef] [PubMed] [Google Scholar]
- National AIDS Control Organization HIV Sentinel Surveillance Report-(HSS-2017) Executive Summary.
- [Google Scholar]
- Spectrum of Cerebrospinal Fluid in Various Stages of Human Immunodeficiency Virus Infection. Arch Neurol. 1988;45:954-8.
- [CrossRef] [PubMed] [Google Scholar]
- Early Penetration of the Blood Brain Barrier by HIV. Neurology. 1988;38:9-14.
- [CrossRef] [PubMed] [Google Scholar]
- Cerebrospinal Fluid in Diseases of the Nervous System (2nd ed). Philadelphia, PA: W.B. Saunders; 1992.
- [Google Scholar]
- Acute Encephalopathy Coincident with Seroconversion for Anti-HTLV-III. Lancet. 1985;2:1206-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neurologic Manifestations of AIDS. Medicine (Baltimore). 1987;66:407-37.
- [CrossRef] [PubMed] [Google Scholar]
- Chemokines and Their Receptors in the Central Nervous System. Front Neuroendocrinol. 2001;22:147-84.
- [CrossRef] [PubMed] [Google Scholar]
- Viral Load in HIV-Associated Dementia. Ann Neurol. 1998;44:150-1.
- [CrossRef] [PubMed] [Google Scholar]
- Pathobiology of Human Immunodeficiency Virus Dementia. Semin Neurol. 1999;19:113-27.
- [CrossRef] [PubMed] [Google Scholar]
- Changes to AIDS Dementia Complex in the Era of Highly Active Antiretroviral Therapy. AIDS. 1999;13:1249-53.
- [CrossRef] [PubMed] [Google Scholar]
- The Dana Consortium on Therapy for HIV Dementia and Related Cognitive Disorders. Neurology. 1996;47:1247-53.
- [CrossRef] [PubMed] [Google Scholar]
- HIV in the Brain: RNA Levels and Patterns of Zidovudine Resistance. Neurology. 2001;57:1396-401.
- [CrossRef] [PubMed] [Google Scholar]
- Scale-up of HIV Treatment Through PEPFAR:A Historic public health Achievement. J Acquir Immune Defic Syndr. 2012;60:S96-S104.
- [CrossRef] [PubMed] [Google Scholar]
- Guidelines for the Use of Antiretroviral Agents in HIV-1-Infected Adults and Adolescents. Available from: https://www.aidsinfo.nih.gov/guidelines/adult/AA_030204.pdf4 [Last accessed on 2013 May 04]
- [Google Scholar]
ANNEXURE